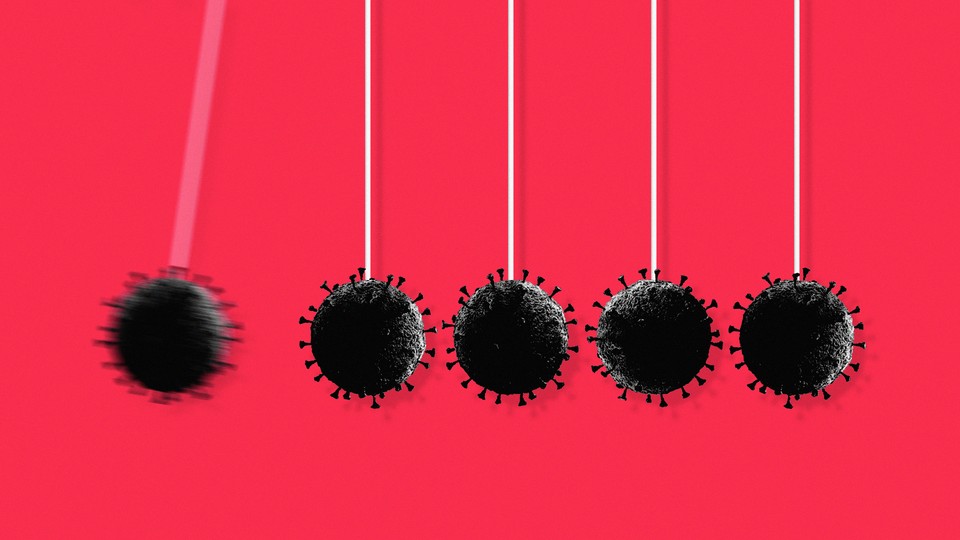
¿Saltó el coronavirus dos veces de los animales a las personas?
Un análisis preliminar de los genomas víricos indica que la pandemia de COVID-19 podría tener múltiples orígenes animales, aunque los resultados aún deben ser revisados por expertos.
Si se confirman con nuevos análisis, los resultados respaldarían la hipótesis de que la pandemia se originó en múltiples mercados de Wuhan, y harían menos probable la hipótesis de que el SARS-COV-2 se escapó de un laboratorio, apuntan algunos investigadores. De todos modos, los datos deben ser verificados, y el análisis aún no ha sido revisado por expertos.
Las primeras secuencias víricas, correspondientes a personas infectadas a finales de 2019 y principios de 2020, se dividen en dos linajes amplios, conocidos como A y B, que presentan algunas diferencias genéticas clave.
El linaje B se ha convertido en el predominante a escala mundial e incluye muestras tomadas de personas que visitaron el mercado de mariscos de Huanan en Wuhan, que también vendía animales silvestres. El linaje A se extendió dentro de China, e incluye muestras de personas vinculadas a otros mercados de Wuhan.
Una cuestión crucial estriba en la relación que existe entre los dos linajes víricos. Si los virus del linaje A evolucionaron a partir de los del linaje B, o viceversa, ello indicaría que el «progenitor» del virus saltó una sola vez de los animales a las personas. Pero si los dos linajes tienen orígenes separados, entonces podría haber habido múltiples eventos de saltos entre especies.
Golpe de gracia
El último análisis, publicado en el foro de discusión virological.org, apunta a la segunda posibilidad al poner en duda la existencia de genomas que vinculen ambos linajes entre sí.
El hallazgo podría ser «el golpe de gracia» a la hipótesis de que el SARS-CoV-2 se escapó de un laboratorio, en lugar de originarse en el mercado de animales salvajes, explica Robert Garry, virólogo de la Universidad de Tulane, en Nueva Orleans (Luisiana). Pero otros afirman que se necesitan más estudios, sobre todo teniendo en cuenta los escasos datos genómicos de los que se dispone de los primeros momentos de la pandemia.
«Es un trabajo muy notable», opina Garry. «Si se demuestra que los linajes A y B son independientes y que hubo dos saltos, casi se puede descartar la idea de que se originó en un laboratorio.»
Los resultados «concuerdan con la existencia de al menos dos introducciones del SARS-CoV-2 en la población humana», afirma David Robertson, virólogo de la Universidad de Glasgow.
Los linajes A y B se caracterizan por dos diferencias clave en los nucleótidos. Pero algunos de los primeros genomas presentan una combinación de estas diferencias. Inicialmente se pensó que estos genomas podrían corresponder a virus de etapas intermedias de la evolución de un linaje a otro.
Pero los autores del nuevo análisis los examinaron en detalle y advirtieron algunas incoherencias.
¿Genomas intermedios?
Al analizar 1716 genomas del SARS-CoV-2 recopilados antes del 28 de febrero de 2020 y procedentes de un repositorio de genomas en línea llamado GISAID, identificaron 38 de estos genomas «intermedios».
Pero cuando examinaron las secuencias con más detalle, descubrieron que muchas de ellas también contenían mutaciones en otras regiones del genoma. Y afirman que estas mutaciones se asocian claramente o bien al linaje A, o bien al B, lo que desacredita la idea de que los genomas víricos correspondientes corresponden a una etapa intermedia de la evolución entre ambos linajes.
Los autores proponen que probablemente se produjo un error de laboratorio o informático al secuenciar una de las dos mutaciones de estos genomas «intermedios». «Cuanto más indagábamos, más nos parecía que no podíamos confiar en ninguno de los genomas de «transición», explica el coautor del estudio Michael Worobey, biólogo evolutivo de la Universidad de Arizona.
Estos errores de secuenciación no son inusuales, dicen los investigadores. A veces, el software puede rellenar los huecos de los datos brutos con secuencias incorrectas, o las muestras víricas pueden contaminarse, señala Richard Neher, biólogo computacional de la Universidad de Basilea. «Estos percances no son de extrañar», afirma. «Especialmente al principio de la pandemia, cuando los protocolos no estaban muy establecidos y se intentaba generar datos lo más rápido posible.»
Varios de los investigadores que secuenciaron algunas de las muestras incluidas en ese estudio afirman que es poco probable que sus secuencias incluyeran errores en los dos nucleótidos clave. Pero los autores del presente estudio replican que, aunque algunos de los genomas se secuenciaran correctamente, otras partes de los mismos genomas, o los lugares donde se obtuvieron las muestras, siguen indicando claramente que pertenecen a uno u otro linaje.
«Resulta muy improbable» que cualquiera de los llamados genomas intermedios sean en realidad genomas de transición, comenta el coautor del estudio Joel Wertheim, epidemiólogo molecular de la Universidad de California en San Diego.
Xiaowei Jiang, bióloga evolutiva de la Universidad Xi'an Jiaotong-Liverpool, en Suzhou (China), afirma que el equipo responsable del estudio debe verificar los resultados obteniendo «los datos originales de secuenciación en bruto de tantos genomas como sea posible».
Varios mercados
Si el virus saltó entre animales y personas en varias ocasiones, el hecho de que los linajes A y B estén vinculados a personas que visitaron diferentes mercados en Wuhan indica que se habrían transportado por la ciudad múltiples animales (de una o más especies) portadores de un «progenitor» del SARS-CoV-2 que habrían infectado a las personas en al menos dos lugares.
Un estudio publicado el pasado junio descubrió que en numerosos mercados de Wuhan se vendían animales vivos vulnerables al SARS-CoV-2, como perros mapaches y visones. Estudios anteriores sobre el virus que causó el síndrome respiratorio agudo severo (SARS) han concluido que también es probable que saltara varias veces de los animales a las personas.
El último trabajo, si se verifica, significaría que la posibilidad de que un investigador infectado accidentalmente en un laboratorio, y que luego propagara el virus a la población general, tendría que haber ocurrido dos veces, explica Garry. Es mucho más probable que la pandemia se originara por el comercio de animales salvajes, afirma.
Para reunir más pruebas, el equipo que ha realizado el nuevo análisis prevé realizar simulaciones por ordenador para comprobar hasta qué punto los contagios múltiples encajarían con la diversidad de los genomas conocidos del SARS-CoV-2.
Smriti Mallapaty/Nature News
Artículo traducido y adaptado por Investigación y Ciencia con el permiso de Nature Research Group.
Encuentra aquí todos los contenidos de Investigación y Ciencia sobre la pandemia de COVID-19. También puedes acceder a los artículos publicados por Scientific American y otras de sus ediciones internacionales a través de esta web.
The Coronavirus Is Here Forever. This Is How We Live With It.
Es de la aparición del SARS-CoV-2, que causa COVID-19, sólo cuatro coronavirus conocidos circulaban entre los humanos, incluyendo 229E. Estos cuatro coronavirus causan resfriados comunes, y en el escenario más optimista, me han dicho los expertos, nuestro nuevo coronavirus terminará siendo el quinto. En ese caso, el COVID-19 podría parecerse mucho a un resfriado de 229E—recurrente pero en gran medida poco destacable," informó Sarah Zhang en agosto.
The Coronavirus Is Here Forever. This Is How We Live With It.
We can’t avoid the virus for the rest of our lives, but we can minimize its impact.
In the 1980s, doctors at an English hospital deliberately tried to infect 15 volunteers with a coronavirus. COVID-19 did not yet exist—what interested those doctors was a coronavirus in the same family called 229E, which causes the common cold. 229E is both ubiquitous and obscure. Most of us have had it, probably first as children, but the resulting colds were so mild as to be unremarkable. And indeed, of the 15 adult volunteers who got 229E misted up their nose, only 10 became infected, and of those, only eight actually developed cold symptoms.
The following year, the doctors repeated their experiment. They tracked down all but one of the original volunteers and sprayed 229E up their nose again. Six of the previously infected became reinfected, but the second time, none developed symptoms. From this, the doctors surmised that immunity against coronavirus infection wanes quickly and reinfections are common. But subsequent infections are milder—even asymptomatic. Not only have most of us likely been infected with 229E before, but we’ve probably been infected more than once.
This tiny study made little impression at the time. In the ’80s and ’90s, coronaviruses still belonged to the backwater of viral research, because the colds they caused seemed trivial in the grand scheme of human health. Then, in the spring of 2020, scientists urgently searching for clues to immunity against a novel coronavirus rediscovered this decades-old research. Before the emergence of SARS-CoV-2, which causes COVID-19, only four known coronaviruses were circulating among humans, including 229E. All four of these coronaviruses cause common colds, and in the most optimistic scenario, experts have told me, our newest coronavirus will end up as the fifth. In that case, COVID-19 might look a lot like a cold from 229E—recurrent but largely unremarkable.
That future may be hard to imagine with intensive-care units filling up yet again during this Delta surge. But the pandemic will end. One way or another, it will end. The current spikes in cases and deaths are the result of a novel coronavirus meeting naive immune systems. When enough people have gained some immunity through either vaccination or infection—preferably vaccination—the coronavirus will transition to what epidemiologists call “endemic.” It won’t be eliminated, but it won’t upend our lives anymore.
With that blanket of initial immunity laid down, there will be fewer hospitalizations and fewer deaths from COVID-19. Boosters can periodically re-up immunity too. Cases may continue to rise and fall in this scenario, perhaps seasonally, but the worst outcomes will be avoided.
We don’t know exactly how the four common-cold coronaviruses first came to infect humans, but some have speculated that at least one also began with a pandemic. If immunity to the new coronavirus wanes like it does with these others, then it will keep causing reinfections and breakthrough infections, more and more of them over time, but still mild enough. We’ll have to adjust our thinking about COVID-19 too. The coronavirus is not something we can avoid forever; we have to prepare for the possibility that we will all get exposed one way or another. “This is something we’re going to have to live with,” says Richard Webby, an infectious-disease researcher at St. Jude. “And so long as it’s not impacting health care as a whole, then I think we can.” The coronavirus will no longer be novel—to our immune systems or our society.
Endemicity as the COVID-19 endgame seems quite clear, but how we get there is less so. In part, that is because the path depends on us. As my colleague Ed Yong has written, the eventuality of endemic COVID-19 does not mean we should drop all precautions. The more we can flatten the curve now, the less hospitals will become overwhelmed and the more time we buy to vaccinate the unvaccinated, including children. Letting the virus rip through unvaccinated people may get us to endemicity quickest, but it will also kill the most people along the way.
The path to endemic COVID-19 will also depend on how much the virus itself continues to mutate. Delta has already derailed summer reopening plans in the U.S. And with so much of the world still vulnerable to infection, the virus has many, many opportunities to luck into new variants that may yet enhance its ability to spread and reinfect. The good news is this virus is unlikely to evolve so much that it sets our immunity back to zero. “Our immune responses are so complex, it’s basically impossible for a virus to escape them all,” says Sarah Cobey, an evolutionary biologist at the University of Chicago. For example, levels of antibodies that quickly neutralize SARS-CoV-2 do indeed drop over time, as happens against most pathogens, but reserves of B cells and T cells that also recognize the virus lie in wait. This means that immunity against infection may wane first, but the protection against severe illness and death are much more durable.
Protection against severe illness and death was, in fact, the original goal of vaccines. When I spoke with vaccine experts as the trials were under way last summer, they universally told me to temper expectations. Vaccines against respiratory viruses rarely protect against full infection because they are better at inducing immunity in the lungs than in the nose, where respiratory viruses gain their first foothold. (Consider: The flu shot is 10 to 60 percent effective depending on the year.) But “the extraordinary efficacy” from the initial clinical trials raised expectations, Ruth Karron, the director of the Center for Immunization Research at Johns Hopkins University, told me. With the Pfizer and Moderna vaccines 95 percent effective against symptomatic infection, eliminating COVID-19 locally, like measles or mumps in the U.S., suddenly seemed possible.
Then came the less pleasant surprise: new variants, like Beta, Gamma, and now Delta, that erode some protection from vaccines. “We now are where we thought we would be a year ago,” Karron said. The vaccines still protect against serious illness very well, as expected, but herd immunity again seems out of reach. The virus will continue to circulate, but fewer people will get sick enough to be hospitalized or die. Highly publicized outbreaks among vaccinated people, such as in Provincetown, Massachusetts, already show this pattern playing out. And entire countries with high vaccination rates, such as the U.K., Iceland, and Israel, are also seeing spikes with only a fraction of their pre-vaccine deaths.
The timing and severity of reinfections and breakthrough infections once COVID-19 becomes endemic depend on how quickly the protective effects of immunity against the virus wanes. And that, in turn, depends on a combination of two factors: first, how quickly our immune systems get rusty against SARS-CoV-2, and second, how quickly this coronavirus evolves to disguise itself. The immunological machinery is simply harder to rouse against an old enemy. But a reinfection or breakthrough infection does reinvigorate the immune response. A breakthrough case acts “like a booster for the vaccine,” as Laura Su, an immunologist at the University of Pennsylvania, told my colleague Katherine J. Wu. In the 229E study, the doctors also found that the volunteers who did not get infected the first time were more likely to be infected when exposed a year later, compared with volunteers who got sick the first time—suggesting that more recent illness is more protective.
The virus itself will also change with time. As more people gain immunity via either infection or vaccination, the coronavirus will try to find ways to evade that immunity too. This is a natural consequence of living with a circulating virus; the flu also mutates every year in response to existing immunity. But in the endemic scenario, where many people have some immunity, the coronavirus will not be able to infect as many people or replicate as many times in each person it infects. “I’m very confident that the rate of adaptation is going to be set by the prevalence of SARS-CoV-2 in the world,” Cobey says. You might think of viral replication as buying lottery tickets, in which the virus accumulates random mutations that very occasionally help it spread. And the fewer lottery tickets the virus has, the less likely it is to hit the mutation jackpot. The appearance of troubling new variants may slow down.
Reinfections with the four common coronaviruses are likely driven by a combination of our immunity fading and the viruses themselves evolving. Putting together everything we do know, a pattern starts to emerge: We are likely first exposed to these common coronaviruses as children, when the resulting disease tends to be mild; our immune systems get rusty; the virus changes; we get reinfected; the immune response is updated; the immune system gets rusty again; the virus changes again; we get infected. And so on.
In the best case, COVID-19 will follow the same pattern, with subsequent infections being mild, says Stephen Morse, an epidemiologist at Columbia University. “If the burden of disease is not high, we take [the virus] very much for granted,” he says. Still, these colds are not completely benign; one of the common-cold coronaviruses has caused deadly outbreaks in nursing homes before. In a less good scenario, COVID-19 looks like the flu, which kills 12,000 to 61,000 Americans a year, depending on the season’s severity. But deaths alone do not capture the full impact of COVID-19. “A big question mark there is long COVID,” says Yonatan Grad, an immunologist and infectious-disease researcher at Harvard. There are still no data to prove how well the vaccines prevent long COVID, but experts generally agree that a vaccinated immune system is better prepared to fight off the virus without doing collateral damage.
The transition to endemic COVID-19 is also a psychological one. When everyone has some immunity, a COVID-19 diagnosis becomes as routine as diagnosis of strep or flu—not good news, but not a reason for particular fear or worry or embarrassment either. That means unlearning a year of messaging that said COVID-19 was not just a flu. If the confusion around the CDC dropping mask recommendations for the vaccinated earlier this summer is any indication, this transition to endemicity might be psychologically rocky. Reopening felt too fast for some, too slow for others. “People are having a hard time understanding one another’s risk tolerance,” says Julie Downs, a psychologist who studies health decisions at Carnegie Mellon University.
With the flu, we as a society generally agree on the risk we were willing to tolerate. With COVID-19, we do not yet agree. Realistically, the risk will be much smaller than it is right now amid a Delta wave, but it will never be gone. “We need to prepare people that it’s not going to come down to zero. It’s going to come down to some level we find acceptable,” Downs says. Better vaccines and better treatments might reduce the risk of COVID-19 even further. The experience may also prompt people to take all respiratory viruses more seriously, leading to lasting changes in mask wearing and ventilation. Endemic COVID-19 means finding a new, tolerable way to live with this virus. It will feel strange for a while and then it will not. It will be normal.
The Atlantic’s COVID-19 coverage is supported by grants from the Chan Zuckerberg Initiative and the Robert Wood Johnson Foundation.
No hay comentarios:
Publicar un comentario