Coronavirus research updates: One nation shows wildly disparate local infection rates
8 July — One nation shows wildly disparate local infection rates
Europe’s largest effort to identify people who have been infected by the new coronavirus has found that roughly one-third of them did not show symptoms.
Between 27 April and 11 May, Marina Pollán at the Institute of Health Carlos III in Madrid and her colleagues tested more than 61,000 people from randomly selected households across Spain for SARS-CoV-2 antibodies, which are produced by the body’s immune system in response to coronavirus infection (M. Pollán et al. Lancet http://doi.org/gg332t; 2020). The study reported large geographical variations in the prevalence of antibodies: more than 10% of people in central areas such as Madrid tested positive, compared with less than 3% in most coastal provinces.
Nationwide, some 5% of people tested positive, of which around one in three were asymptomatic. On the basis of their results, the researchers estimate that roughly one million people previously infected with the coronavirus could have gone undetected in Spain because they did not show symptoms.
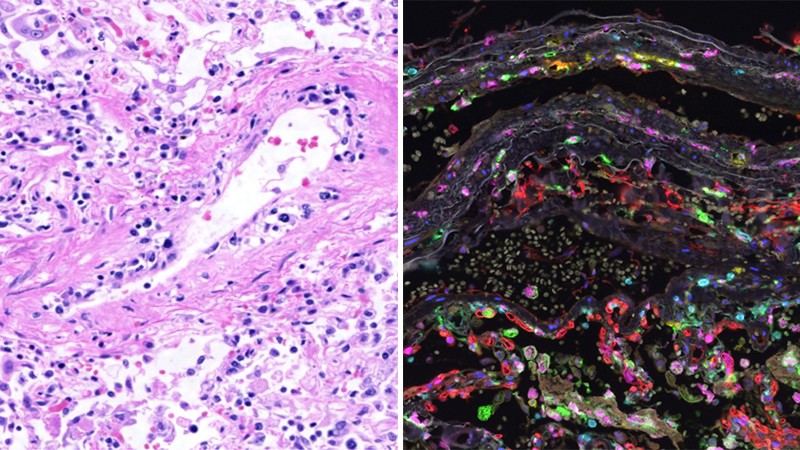
7 July — Autopsies links immune response to death from COVID-19
An autopsy-based study of 11 people who died from COVID-19 shows a mismatch between viral hotspots in the body and sites of inflammation and organ damage, suggesting that immune responses, rather than the virus itself, are responsible for death.
Numerous studies have suggested that the immune system contributes to the organ damage seen in some severe cases of COVID-19. Christopher Lucas and David Dorward at the University of Edinburgh, UK, and their colleagues conducted detailed autopsies to map signs of SARS-CoV-2 in the body, along with sites of inflammation and injury (D. A. Dorward et al. Preprint at medRxiv http://doi.org/d27t; 2020).
The survey of 37 anatomical sites, including the lungs, found little correlation between levels of the virus and inflammation: some tissues harboured the virus but were not inflamed, whereas others were damaged but did not contain high levels of SARS-CoV-2. The findings have not yet been peer reviewed.
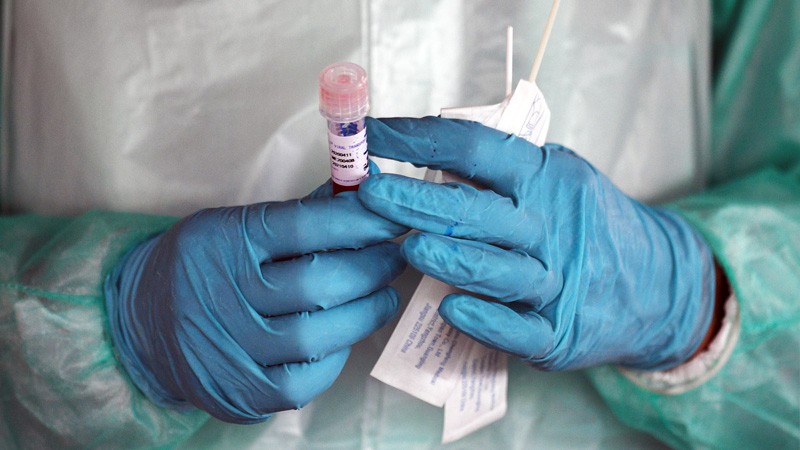
26 June — Test frequency matters more than test sensitivity for stopping outbreaks
Communities such as universities where COVID-19 cases could quickly spiral out of control should frequently test large numbers of people for the new coronavirus — even if that means using a relatively insensitive test.
Tests that rely on the technique quantitative polymerase chain reaction (qPCR) can detect the merest traces of SARS-CoV-2 genetic material but are expensive and slow to return results. To gauge the importance of test sensitivity, Michael Mina at the Harvard T. H. Chan School of Public Health in Boston, Massachusetts, and his colleagues modelled the effect of widespread testing on viral spread in a large group of people (D. B. Larremore et al. Preprint at medRxiv, http://doi.org/d2gt; 2020).
The researchers found that weekly surveillance testing, paired with case isolation, would limit an outbreak even if the testing method was less sensitive than qPCR. By contrast, surveillance testing done every 14 days would allow the total number of infections to climb almost as high as if there were no testing at all. The findings have not yet been peer reviewed.
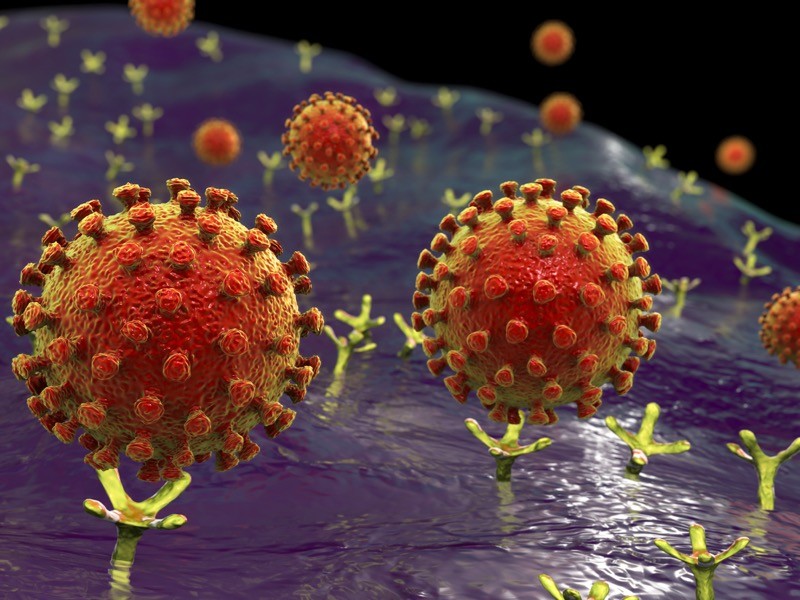
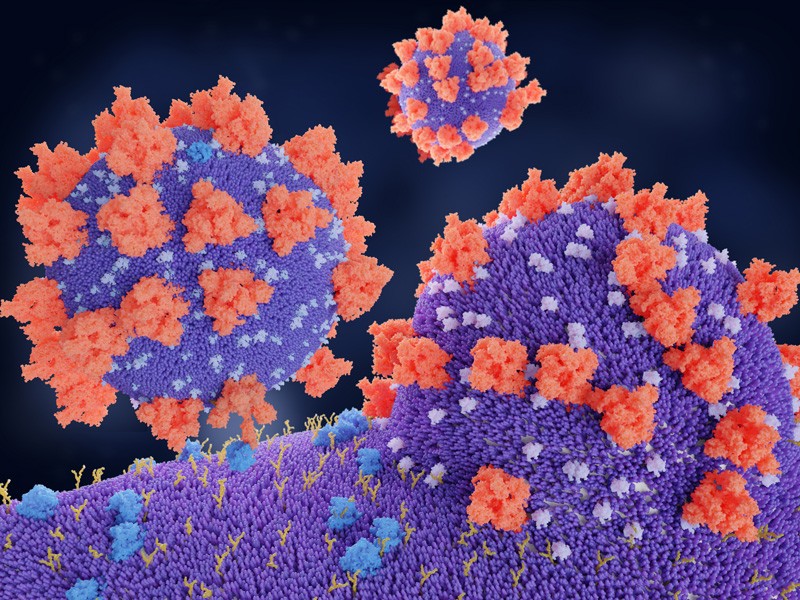
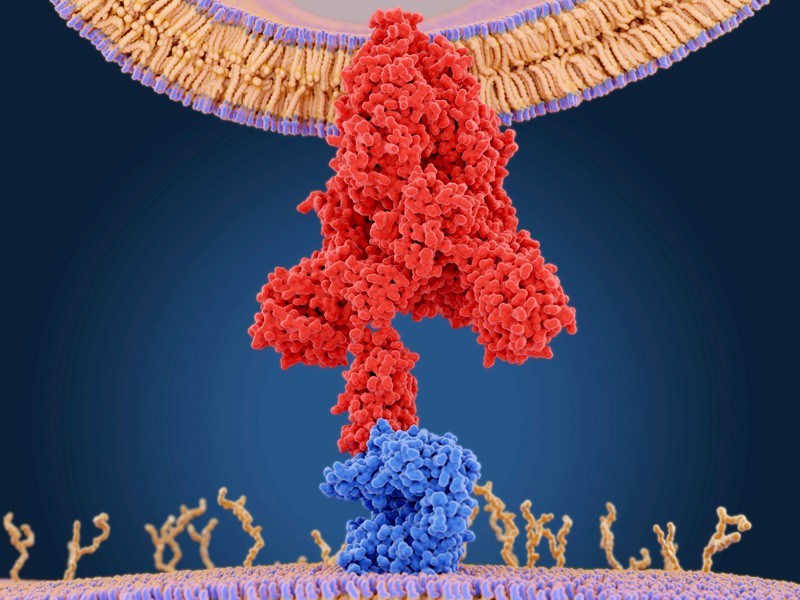
24 June — A finely detailed map reveals a viral protein’s Achilles heel
Scientists have created and described more than 3,800 variations of the protein that the new coronavirus uses to latch on to its targets — a feat that reveals which parts of the protein are crucial for binding to human cells.
Before SARS-CoV-2 invades a cell, a viral protein called spike fastens tightly to a receptor that sits on the surface of many human cells. Jesse Bloom at the Fred Hutchinson Cancer Research Center in Seattle, Washington, and his colleagues altered a single amino acid at a time in a key segment of spike to produce 3,804 variants of the protein (T. N. Starr et al. Preprint at bioRxiv http://doi.org/dz8r; 2020). Tests showed that many of these variants bind to the receptor at least as well as the protein in the coronavirus causing the current pandemic.
The tests allowed the team to pinpoint the amino acids that, if altered, impair the spike protein’s binding ability. This knowledge could help researchers to develop molecules that neutralize the virus’s ability to infect cells. The findings have not yet been peer-reviewed.
23 June — A striking share of infected people never show classic symptoms
Less than one-third of people infected with SARS-CoV-2 fell ill with respiratory symptoms or fever, according to a survey of thousands of people in Italy.
More than 16,000 people in Lombardy have died of COVID-19, making the region the epicentre of Italy’s coronavirus outbreak. Piero Poletti at the Bruno Kessler Foundation in Trento, Italy, Marcello Tirani at the Health Protection Agency of Pavia in Italy and their colleagues studied people in Lombardy who had had close contact with an infected person.
Roughly half of these 5,484 contacts became infected themselves (P. Poletti et al. Preprint at https://arxiv.org/abs/2006.08471; 2020). Of those, 31% developed respiratory symptoms — such as a cough — or a fever; only 26% of those under the age of 60 did so. As a person’s age increased, so did their odds of experiencing symptoms and becoming ill enough to require intensive care, or to die. The results could inform hospitals’ outbreak preparations, the authors say.
The findings have not yet been peer reviewed.
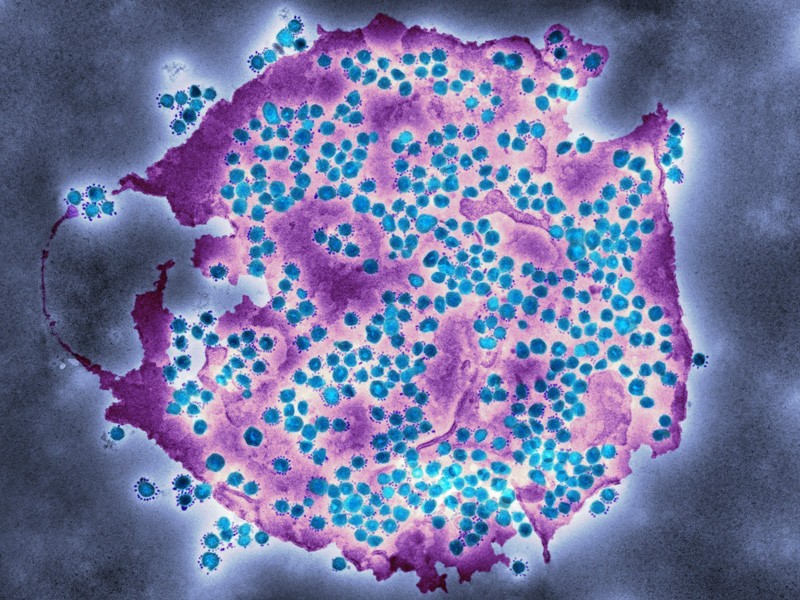
22 June — CRISPR pinpoints host genes that aid viral invasion
A trawl through a monkey genome using the CRISPR–Cas9 genome-editing system has identified a handful of genes that might help the new coronavirus to infect its hosts.
The discovery of host genes that aid viral activity could aid the development of new therapies, and reveal why some people are more susceptible to COVID-19 than others. John Doench at the Broad Institute of MIT and Harvard in Cambridge, Massachusetts, Craig Wilen at Yale School of Medicine in New Haven, Connecticut, and their colleagues used CRISPR–Cas9 to alter genes in cultured monkey cells. They then looked for those genes that influenced viral infection and host-cell death (J. Wei et al. Preprint at bioRxiv http://doi.org/dzz3; 2020).
The team’s survey found genes that code for several proteins not known to assist the coronavirus. Among them are proteins in the TGF-β signalling pathway, which is involved in cell growth and death. Chemicals that inhibit this pathway also prevented coronavirus-induced cell death. The findings have not yet been peer reviewed.
19 June — Youth is a shield against infection by close contacts
People under the age of 20 are much less likely than their elders to catch the new coronavirus from an infected household member.
Yang Yang at the University of Florida, Gainesville, Zhi-Cong Yang at the Guangzhou Center for Disease Control and Prevention in China and their colleagues analysed viral transmission between infected people in Guangzhou and those who’d had close contact with them (Q. Jing et al. Lancet Inf. Dis. http://doi.org/dznw; 2020). After public-health officials had instituted isolation of infected individuals and quarantine of their contacts, people under the age of 20 had a 5.2% risk of being infected by a member of their household, compared with a 14.8% risk for people aged 20–59 and an 18.4% risk for people aged 60 and above.
The researchers also found that people with COVID-19 were at least as infectious before their symptoms started as after. The authors suggest that viral spread within households could be limited by providing facilities where infected people could isolate themselves from their families.
17 June — More than one billion people face increased risk of severe COVID-19
A host of common health problems boost a person’s risk of becoming seriously ill if infected by the new coronavirus. Now an analysis reveals the extent of this vulnerable group: more than 20% of the world’s population has at least one underlying condition that raises the risk of severe disease.
Andrew Clark at the London School of Hygiene & Tropical Medicine and his colleagues examined the prevalence of diabetes, cardiovascular problems and other conditions that predispose people infected with SARS-CoV-2 to severe COVID-19 (A. Clark et al. Lancet Glob. Health http://doi.org/dzk9; 2020). Analysing data from 188 nations, the team estimates that 1.7 billion people worldwide have an elevated risk of ‘severe’ illness. The researchers also estimate that nearly 350 million people — some of whom do not have underlying conditions — would require hospitalization if infected.
These findings can be used to assess how many high-risk people will need a vaccine once it is developed, the authors say.
16 June — Swiss survey finds that children are less susceptible to infection
Children and the elderly are less likely than adults under the age of 65 to show evidence of past SARS-CoV-2 infection, according to a survey of people in Geneva, Switzerland.
Silvia Stringhini at Geneva University Hospitals and her colleagues tested some 2,700 people aged 5 and older for antibodies produced by the immune system to prevent reinfection with the new coronavirus (S. Stringhini et al. Lancet http://doi.org/dzh5; 2020).
The researchers found that only one out of the 123 children aged 5–9 tested positive, although 21 of them lived with someone who had COVID-19 antibodies. Of 369 participants aged 65 or older, 11 lived with another person with COVID-19 antibodies and 15 tested positive.
The researchers say that the low prevalence for children suggests that they might be less susceptible to infection, whereas the low prevalence in the elderly might stem from less exposure to the virus and an ageing immune response.
15 June — Bars, karaoke and gyms can aid ‘superspread’
Clusters of coronavirus infections are often linked to events many people breathe heavily while packed together, such as karaoke parties and and gym sessions, according to a survey in Japan.
Hitoshi Oshitani at Tohoku University in Sendai, Japan, and his colleagues analysed clusters of at least five infected people who had all attended the same event or venue (Y. Furuse et al. Emerg. Inf. Dis. http://doi.org/ggz2hg; 2020). Many of the 61 ‘superspreading’ incidents they identified occurred in hospitals, nursing homes and other care facilities, but a little more than half took place at venues such as musical events, restaurants and workplaces.
One concert, for example, was the source of infection for more than 30 people, including performers, audience members and staff.
The team identified the probable founders of 22 of the superspreading events, and the timing for 16 of them. The results showed that half of the superspreading individuals were under the age of 40, and 41% had had no symptoms when they transmitted the virus.
12 June — Modified mice could aid the quest for vaccines and drugs
Two teams have developed a short cut to generating COVID-19 mouse models: using a harmless virus to make the rodents cells susceptible to infection.
The SARS-CoV-2 virus invades a human cell by attaching to receptors, including one called ACE2, on its surface. Mice have a different version of ACE2, making them impervious to SARS-CoV-2 infection. Transgenic mice carrying the human version of ACE2 are susceptible to infection but are scarce.
To develop a more widely available mouse model, a team led by Michael Diamond at Washington University in St. Louis, Missouri, and another by Jincun Zhao at the First Affiliated Hospital of Guangzhou Medical University in China used adenoviruses — a workhorse of gene therapy — to deliver the human ACE2 gene to the lung cells of mice. After exposure to SARS-CoV-2, these mice lost weight and developed pneumonia.
Diamond’s team successfully treated the ill mice with therapeutic antibodies (A. O. Hassan et al. Cell http://doi.org/dzbk; 2020). Zhao’s group used the mice to test an experimental vaccine and several therapies for COVID-19 (J. Sun et al. Cell http://doi.org/dzbm; 2020).
11 June — A massive number of viral imports seeded the UK outbreak
The new coronavirus has jumped into the United Kingdom more than 1,300 times — mostly from France and Spain, despite early headlines focusing on infected travellers from China and other parts of Asia.
COVID-19 has killed more than 40,000 people in the United Kingdom. To understand the origins of the outbreak there, a team led by Oliver Pybus at the University of Oxford, UK, and Andrew Rambaut at the University of Edinburgh, UK, analysed nearly 30,000 SARS-CoV-2 genomes (O. Pybus et al. Preprint at Virological https://go.nature.com/37ieyvw; 2020).
The team tracked the number of times the virus reached the United Kingdom and began to spread inside the country’s borders. Genomic analysis found that there were 1,356 such introductions, although the researchers say that this number is preliminary and probably an underestimate.
Travellers from Spain accounted for roughly one-third of those introductions, and travellers from France slightly less than one-third. People coming from China accounted for less than 0.1% of introductions. The findings have not yet been peer reviewed.
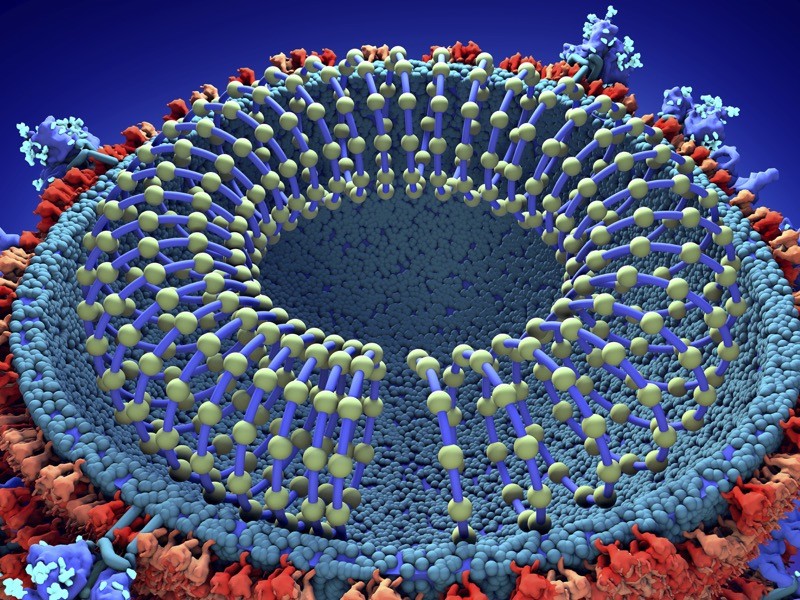
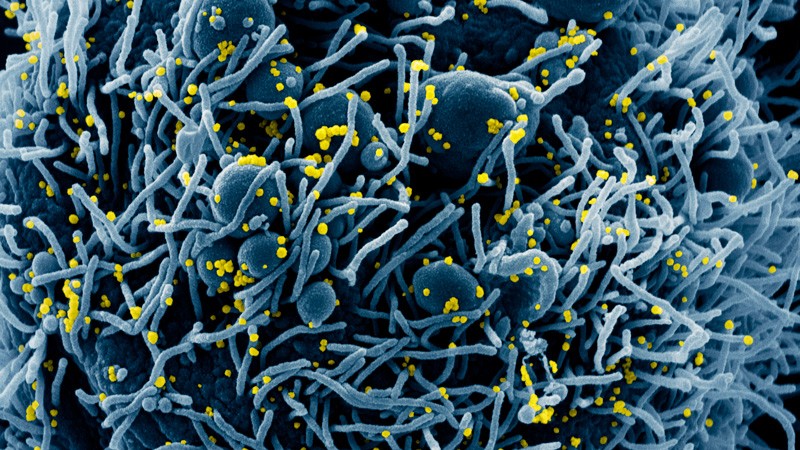
11 June — Virus conscripts a pair of human proteins to invade cells
Researchers have found a second protein that SARS-CoV-2 uses to enter human cells, potentially offering a new target for vaccines and drugs.
The SARS-CoV-2 protein called Spike is known to attach to a human protein called ACE2, which allows the virus to enter cells. Two teams of researchers have now found that the human protein neuropilin-1 (NRP1) also aids viral invasion.
Peter Cullen and Yohei Yamauchi at the University of Bristol, UK, and their colleagues showed that a fragment of the Spike protein can bind to NRP1 (L. Cantuti-Castelvetri et al. Preprint at bioRxiv http://doi.org/dx5c; 2020). Both this team’s findings and those of Mikael Simons at the Technical University of Munich, Germany, and his colleagues (J. L. Daly et al. Preprint at bioRxiv http://doi.org/dx5d; 2020) show that an antibody that binds to NRP1 can block infection of human cells grown in the laboratory.
The Simons team also found that in mice, NRP1 assists the entry of virus-sized particles into the central nervous system. The studies suggest that blocking the interaction between the virus and NRP1 could provide a way to combat coronavirus infection.
Neither study has been peer reviewed yet.
9 June — People who feel fine can unknowingly spread the virus
A massive coronavirus testing campaign in Vietnam has found evidence that infected people who never show any symptoms can pass the virus to others.
Early in the global COVID-19 outbreak, Vietnam began to repeatedly test people at high risk of infection. Those who tested positive were admitted to a hospital until they either recovered or tested negative.
Of roughly 14,000 people tested between mid-March and early April, 49 were infected. Le Van Tan at the Oxford University Clinical Research Unit in Ho Chi Minh City, Vietnam, and his colleagues monitored 30 of the 49 individuals and found that 13 developed no symptoms during their hospital stay (N. V. V. Chau et al. Clin. Infect. Dis. http://doi.org/ggzfz9; 2020).
Nasal swabbing showed that the infected but asymptomatic study participants had lower levels of viral RNA than infected people who felt ill at some point. But it’s “highly likely” that two of the asymptomatic participants were the source of infection for at least two other people, the authors say.
8 June— Lockdowns are a powerful tool against the pandemic
Lockdowns and other distancing measures have had resounding success at thwarting the new coronavirus, according to two independently conducted studies that examined different countries and measures of effectiveness.
Samir Bhatt at Imperial College London and his colleagues used data on COVID-19-related deaths to model viral transmission in 11 European countries (S. Flaxman et al. Nature http://doi.org/dxxs; 2020). The team found that in those nations, the combination of policies aimed at slowing the virus’s spread prevented more than 3 million deaths from the epidemic’s start to early May.
In each country, the actions taken were enough to halt the epidemic. Lockdowns — stay-at-home orders and policies that restrict face-to-face contact — were especially effective, reducing transmission by 81%.
Solomon Hsiang at the University of California, Berkeley, and his colleagues analysed how the growth rate of infections changed over time in China, the United States and four more countries that applied policies to prevent viral spread (S. Hsiang et al. Nature http://doi.org/dxxt; 2020). The analysis showed that across all 6 countries, anti-transmission measures averted roughly 500 million infections.
This team also found that lockdowns — policies that require people to stay at home whether or not they are infected — are effective at stemming viral spread.
5 June — Surfaces could pose only a modest risk for household spread
Contaminated surfaces might have only a minor role in transmitting COVID-19 within households.
Ricarda Schmithausen at the University of Bonn in Germany and her colleagues looked for traces of the virus SARS-CoV-2 in 21 households that each included at least one infected person (M. Döhla et al. Preprint at medRxiv http://doi.org/dxqn; 2020). The team found viral RNA in just 3% of samples from the most frequently touched objects, such as door knobs, and in 15% of samples taken from bathroom drains and toilets. The team could not grow infectious virus from any of the samples.
All 15 samples from air monitors designed to pick up fine respiratory aerosol particles tested negative for viral RNA, although the authors say that the method they used means this result should be interpreted cautiously.
The findings suggest that direct transmission of the coronavirus, for example through exhaled or coughed droplets, is probably the main route of infection. However, transmission in wastewater is a possible route of infection, the authors add.
The results have not yet been peer reiviewed.
4 June — Blood type might influence COVID-19 risk
Researchers have identified two human gene variants that could make people more susceptible to lung failure associated with COVID-19.
Tom Karlsen at Oslo University Hospital and his colleagues analysed the genomes of roughly 4,000 people from Italy and Spain: 1,980 people with COVID-19 who developed respiratory failure and more than 2,000 people who did not have the disease (D. Ellinghaus et al. Preprint at medRxiv http://doi.org/dxk7; 2020). Those with severe COVID-19 were more likely to carry either of two gene variants than people without the disease.
One variant lies in the swathe of the genome that determines blood groups. A follow-up analysis found that people with blood type A+ had an increased risk of lung failure compared with those with other blood types, whereas those with type O blood were protected to some extent. The study flagged a second variant, on chromosome 3, that is near six genes, including one that interacts with the molecular receptor the virus uses to enter human cells.
The study has not yet been peer-reviewed.
3 June — Drug hailed for its potency fails to prevent infection
A large clinical trial has found no evidence that the drug hydroxychloroquine protects people from COVID-19.
Some world leaders have embraced hydroxychloroquine as a treatment for COVID-19 or as an agent to prevent the disease. David Boulware at the University of Minnesota in Minneapolis and his colleagues randomly assigned 821 people to take either hydroxychloroquine or a placebo within 4 days of exposure to SARS-CoV-2 (D. R. Boulware et al. N. Engl. J. Med. http://doi.org/dxkv; 2020). Some study participants were health-care workers who had contact with infected people; others shared a house with an infected person.
About 12% of people given hydroxychloroquine developed COVID-19 within 2 weeks, compared with about 14% who were given the placebo. That difference is not statistically significant. Those taking the drug also reported more side effects than those taking the placebo.
The authors note an important caveat to the study: tests were not available for people, including health-care workers, unless they had symptoms of COVID-19. Therefore, asymptomatic cases are unaccounted for.
2 June — Could antibody tests downplay virus’s prevalence?
Antibody studies might underestimate the share of a population that has been infected with SARS-CoV-2.
In response to a pathogen attack, immune cells produce molecules called antibodies, which can linger in the blood and provide a record of infection. Isabel Rodríguez-Barraquer at the University of California, San Francisco, and her colleagues identify a potential source of bias in tests that detect the presence of antibodies against the new coronavirus (S. Takahashi et al. Preprint at OSF Preprints http://doi.org/dxc2; 2020).
Most antibody tests have been validated using blood samples from people hospitalized with severe disease. But these individuals, who make up only a small fraction of infected people, might have higher levels of antibodies circulating in their body than have people with mild or no symptoms.
The researchers say more detailed studies are needed to assess how well antibody tests detect previous infection in people who had mild disease.
The findings have not yet been peer reviewed.
1 June — Positive coronavirus test is no guarantee of infectiousness
People with COVID-19 are unlikely to spread the new coronavirus if more than eight days have passed since their symptoms began, according to experiments in monkey cells.
Jared Bullard at the University of Manitoba in Winnipeg, Canada, and his colleagues seeded cultured monkey cells with 90 human samples that had tested positive for SARS-CoV-2 RNA (J. Bullard et al. Clin. Infect. Dis. http://doi.org/dw8z; 2020). The researchers found that RNA-positive samples collected more than eight days after a person’s symptoms began did not infect the cells — suggesting that people who test positive for viral RNA are not necessarily infectious.
Hospital patients who still test positive for viral RNA weeks after they began feeling ill might not need to be strictly isolated, the team says.
29 May — The nose could be the body’s entry point to infection
The nose is the probable starting point for COVID-19 infections.
Richard Boucher and Ralph Baric at the University of North Carolina at Chapel Hill and their colleagues tracked the ease with which the new coronavirus infects various cell types in the respiratory tract. The researchers found a gradient of infectivity that decreases from the upper to the lower respiratory tract: the most easily infected cells are in the nasal cavity, and the least easily infected deep in the lungs. (Y. J. Hou et al. Cell http://doi.org/dw2j; 2020). That gradient mapped neatly onto the distribution of cells that express ACE2, a protein that SARS-CoV-2 uses to enter cells.
The authors speculate that the virus gets a foothold in the nose, then sneaks down the respiratory tract when breathed into the airways. They say the results support the use of masks and preventative measures such as nasal cleansing.
28 May — A lost opportunity to stop viral spread in the United States
Genomic analysis has contradicted a high-profile finding about the origins of the first community spread of the new coronavirus in the United States.
In late February, a widely publicized genomic analysis suggested that SARS-CoV-2 had been silently spreading for weeks in Washington state. The analysis traced the outbreak’s origin to a traveller designated WA1 — even though officials had quickly detected WA1’s infection after his arrival from China on 15 January and had done extensive contact tracing to stop transmission.
But modelling by Michael Worobey at the University of Arizona, Tucson, and his colleagues suggests that WA1 did not trigger a wider outbreak. Instead, the team found evidence that the virus that spread in Washington reached the state from China in mid-February (M. Worobey et al. Preprint at bioRxiv http://doi.org/dwx3; 2020). The findings have not yet been peer-reviewed.
The four weeks between WA1’s arrival and the arrival of the actual source were a “missed opportunity” to stop the virus from taking hold in the United States, the authors say.
27 May — Superspread in Israel caused a high portion of infections
An “extremely high level” of viral superspread helped to seed the new coronavirus across Israel, according to the authors of a genomic analysis.
Adi Stern at Tel Aviv University in Israel and her colleagues sequenced and analysed more than 200 SARS-CoV-2 genomes from people across Israel (D. Miller et al. Preprint at medRxiv http://doi.org/dwvb; 2020). The results, which have not yet been peer-reviewed, show that only 1–10% of infected people caused 80% of the next wave of cases, illustrating the power of superspreaders in viral transmission.
The analysis also found that travelers from the United States and Europe carried the virus to Israel, but US travelers were responsible for a disproportionate share of viral spread. One possible explanation: Israel began restricting entry of people arriving from Europe before it banned US arrivals.
26 May — Exposed children escape infection more often than adults
Children and adolescents under the age of 20 are much less likely than adults to become infected by the new coronavirus, finds a large systematic review of journal articles, preprints and reports.
Russell Viner at University College London and his colleagues screened more than 6,000 studies, of which 18 provided data that met the authors’ criteria for inclusion. The 18 included 7 that had been peer reviewed (R. M. Viner et al. Preprint at medRxiv http://doi.org/dwp6; 2020).
Studies that traced the contacts of infected individuals show that children are 56% less likely to get infected than adults when in contact with an infected person. The analysis suggests that children have played a smaller part than adults in spreading the virus in the population, but the evidence for this finding is weak. There has not been enough research to determine whether infected children are less likely than adults to pass on the infection, the authors conclude.
The study has not yet been peer reviewed.
25 May — Trump’s favoured drug shows no benefit — but another drug does
World leaders, including US President Donald Trump, have touted the antimalarial drug hydroxychloroquine as a treatment for COVID-19. But a study of nearly 100,000 people found no benefit to the drug and linked it instead to an elevated risk of death and abnormal heart rhythms.
Mandeep Mehra at the Brigham and Women’s Hospital Heart and Vascular Center in Boston, Massachusetts, and his colleagues analysed the health records of more than 96,000 people treated for COVID-19. The study drew on data from patients at 671 hospitals on 6 continents (M. R. Mehra et al. The Lancet http://doi.org/ggwzsb; 2020). Roughly 15% of these patients received hydroxychloroquine, the related drug chloroquine, or one or the other of these drugs paired with an antibiotic.
Compared with people who did not take the drugs, people in all four treatment arms were more likely to die in hospital and more likely to develop a disordered heartbeat, or arrhythmia. The authors say that only people enrolled in clinical trials should take the drugs.
A separate trial of the drug remdesivir showed that it shortens the recovery of people hospitalized with COVID-19. John Beigel at the National Institutes of Allergy and Infectious Diseases in Rockville, Maryland, and his colleagues studied more than 1,000 people enrolled in a randomized, double-blind trial and found that those who took remdesivir had a median recovery time of 11 days, compared with 15 days for those who took a placebo (J. H. Beigel et al. N. Engl. J. Med. http://doi.org/dwkd; 2020).
Editors’ note: The Lancet has published a retraction (https://www.thelancet.com/lancet/article/s0140673620313246) of the controversial paper by Mehra et al. on hydroxychloroquine.
22 May — DNA vaccines protect monkeys from coronavirus
Monkeys were protected from the new coronavirus after receiving a DNA vaccine against the virus.
Dan Barouch at Harvard Medical School in Boston, Massachusetts, and his colleagues explored vaccines composed of DNA (J. Yu et al. Science http://doi.org/dwfb; 2020). This type of vaccine prompts the recipient’s cells to make a pathogen or its components. That, in turn, stimulates the immune system.
The researchers developed six DNA vaccines based on a coronavirus protein called spike and tested them in rhesus macaques (Macaca mulatta). The animals mounted an antibody response similar to that seen in macaques and people who had recovered from SARS-CoV-2 infection.
The team then gave doses of coronavirus to the vaccinated monkeys, which developed only mild illness. Viral multiplication in the animals was generally lower than in unvaccinated monkeys, probably because the vaccinated animals’ immune systems kept the virus in check.
21 May — Potent human antibodies could inspire a vaccine
A vaccine typically works by triggering the body’s immune response, which generates antibodies that fend off a particular virus. But some viruses do not stimulate a protective antibody response, which means there’s no guarantee that a vaccine can be developed for every disease.
Davide Robbiani at Rockefeller University in New York City and his colleagues studied 68 people who had recovered from SARS-CoV-2 infection and found that they all had generated varying amounts of antibodies against the virus. A fraction of these antibodies strongly blocked the coronavirus from invading human cells (D. F. Robbiani et al. Preprint at bioRxiv http://doi.org/ggwfcm; 2020). The work has not yet been peer reviewed.
People who’d recovered from severe disease had higher levels of these potent antibodies, on average, than people whose illness was milder. But every participant appeared to be capable of making them. The authors suggest that a vaccine designed to elicit these potent antibodies might be universally effective.
21 May — Monkeys resist re-infection after recovering from the virus
Monkeys that had recovered from infection with the new coronavirus were protected from re-infection, although how long the protection lasts is unclear.
Public-health officials need to know whether people who have been infected with SARS-CoV-2 can be infected again. To address this issue, Dan Barouch at Harvard Medical School in Boston, Massachusetts, and his colleagues gave doses of the coronavirus to nine rhesus macaques (Macaca mulatta). The monkeys developed mild symptoms, such as appetite loss, as well as antibodies against the virus (A. Chandrashekar et al. Science http://doi.org/dwck; 2020).
Roughly one month later, the researches gave the monkeys another dose of virus. Over the following two weeks, the team detected low, rapidly declining levels of viral RNA in the animals’ noses and almost none in the monkeys’ lungs. All of the monkeys mounted an antibody response to the second dose of SARS-CoV-2, suggesting that their immune systems had fought off the virus.
20 May — The virus ravages organs from heart to brain
Autopsies have found the new coronavirus not only in the lungs, but also in the kidneys, heart, brain and other organs.
COVID-19 is principally considered a respiratory disease, but some infected people experience non-respiratory symptoms, such as stroke. Tobias Huber at the University Medical Center Hamburg-Eppendorf in Germany and his colleagues conducted autopsies on 27 people with COVID-19. They found that the virus was most abundant in the lungs, but was also present at lower levels in the kidneys, liver, heart, brain and blood (V. G. Puelles et al. N. Engl. J. Med. http://doi.org/dv56; 2020).
By scrutinizing databases of genetic activity, the team found that three genes known to encourage SARS-CoV-2 infection are highly active in kidney cells. Additional analysis of 6 people detected virus in all examined kidney compartments, which helps to explain the kidney damage seen in some people with the illness.
19 May — An antibody blocks the new coronavirus and an older relative
An antibody discovered in the blood of a person who survived SARS could help others to fight COVID-19.
The coronavirus that caused the 2003 SARS outbreak is a distant relative of SARS-CoV-2, the virus responsible for the current pandemic. The newfound antibody, dubbed S309, recognizes and blocks both viruses, report David Veesler at the University of Washington in Seattle, Davide Corti at Vir Biotechnology in Bellinzona, Switzerland, and their colleagues (D. Pinto et al. Nature https://doi.org/dv4x; 2020).
The antibody is an immune signalling molecule that attaches to a viral protein called spike, which both viruses use to enter human cells. The team’s structural analysis shows that S309 binds to a location on spike that is distinct from the attachment site of some of the person’s other coronavirus-targeted antibodies. Two cocktails, each combining one of these two antibodies with S309, were better at blocking the virus than was each antibody alone.
18 May — Dogs can catch coronavirus from their owners
The first two dogs reported to have coronavirus probably caught the infection from their owners, say researchers who studied the animals and members of the infected households in Hong Kong. An analysis showed that the viral genetic sequences from the dogs were identical to those from the infected people.
The researchers studied 15 dogs who lived with people with COVID-19 (T. H. C. Sit et al. Nature http://doi.org/dvt4; 2020). Only two — a Pomeranian and a German shepherd — caught the disease. The team detected viral RNA and antibodies in both dogs, and live virus in one. Neither dog became noticeably sick.
The study showed no evidence that dogs can pass the infection to other dogs or to people.
15 May — Promising vaccine shields monkeys from lung damage
An experimental COVID-19 vaccine protected monkeys from pneumonia and prompted a strong immune response in the animals.
Vincent Munster at the National Institute of Allergy and Infectious Diseases in Hamilton, Montana, Sarah Gilbert at the University of Oxford, UK, and their colleagues designed a vaccine that encodes the new coronavirus’s spike protein, which it uses to invade host cells (N. van Doremalen et al. Preprint at bioRxiv http://doi.org/dvvd; 2020). The researchers injected 6 rhesus macaques (Macaca mulatta) with the vaccine before giving the animals high doses of virus.
The vaccinated monkeys all developed neutralizing antibodies — which can prevent a virus from entering cells — against SARS-CoV-2. Vaccinated animals had much lower levels of viral RNA in their lung tissue than unvaccinated animals, suggesting that the vaccine stopped the virus from multiplying in the monkeys’ lungs. Two of the three control monkeys developed pneumonia; none of the vaccinated monkeys did. The research has not yet been peer-reviewed.
A clinical trial of the vaccine is now underway.
15 May — Lifting lockdown could spell surge of infections for France
More than 20,000 people in France have died of COVID-19, but the nation’s infection rate in mid-May stood at roughly 5% — well short of the 65% needed for herd immunity.
Simon Cauchemez at the Pasteur Institute in Paris and his colleagues modelled France’s coronavirus outbreak. (H. Salje et al. Science, http://doi.org/dvt3; 2020). They found that France’s lockdown, which began 17 March, reduced viral spread by 77%. The team projected that by the time the lockdown was relaxed on 11 May, an estimated 4.4% of the population would have been infected.
Some two-thirds of the population would need to be immune for immunity alone to control the epidemic. As a result, herd immunity cannot prevent “a second wave at the end of the lockdown”, the authors write.
14 May — ‘Superspread’ at a choir practice infects dozens
A single ill person who attended a choir practice in Washington State led to the probable infection of more than 50 choir members, including 2 who died.
Lea Hamner and her colleagues at Skagit County Public Health in Mount Vernon, Washington, analysed numerous local cases of COVID-like illness and traced them to an evening choir practice on 10 March (L. Hamner et al. Morb. Mortal Wkly. Rep. 69, 606–610; 2020). One symptomatic person attended the 2.5-hour practice and later tested positive for SARS-CoV-2. Of the other 60 people in attendance, 32 became ill with confirmed COVID-19 and an additional 20 became ill with probable infections.
Choir members sat in close-packed rows and sang for long periods, which might have contributed to viral transmission. This superspreading event emphasizes the importance of avoiding crowds and close interactions to keep the virus at bay, the authors say.
14 May — The very youngest children are most likely to enter hospital
Children with COVID-19 are at a lower risk of death than are adults with the disease, according to the largest study of infected children in Europe.
Silvia Garazzino at the University of Turin, Italy, and her colleagues analysed data from children under the age of 18 who turned up at hospitals and clinics with COVID-19 symptoms. All 168 who tested positive for the coronavirus recovered fully (S. Garazzino et al. Preprint at Eurosurveillance http://doi.org/dvk8; 2020). The study has not yet been peer-reviewed.
Nearly 80% of infants under the age of one were hospitalized, compared with 53% of those between the ages of 11 and 17. A national survey estimates that the overall hospitalization rate for infected children in Italy is much lower — around 4%.
Two-thirds of the children had at least one infected parent, whose symptoms often appeared before the child’s did.
13 May — New York City’s infection hotspots have high numbers of commuters
New York City neighbourhoods that were COVID-19 hotspots between March and May correlate with those that were home to the highest number of commuters over the past three months.
To understand why deaths and hospitalizations from COVID-19 varied so substantially between the city’s neighbourhoods, Stephen Kissler at the Harvard T.H. Chan School of Public Health in Boston, Massachusetts, and his colleagues compiled coronavirus test results from about 1,700 women who came to 6 city hospitals to give birth (S. M. Kissler et al. Preprint at https://bit.ly/2Aq7dpb; 2020).
The team analysed the postal codes of infected women to estimate disease prevalence in city neighbourhoods. The researchers then compared this information with location data from Facebook that revealed the number of daily trips that people take into and out of each neighbourhood, and found a link between a neighbourhood’s infection rate and the number of trips taken by its residents.
Many of the commuters are probably ‘essential workers’, who should be protected to prevent the virus’s spread, the authors say.
12 May — The body launches a sweeping antibody response to coronavirus
People infected by the new coronavirus make antibodies against several of the virus’s proteins — a finding that could lead to more effective vaccines and more sensitive tests to determine who has already been infected and might now be immune.
Niloufar Kavian and Sophie Valkenburg at the University of Hong Kong and their colleagues wanted to determine which SARS-CoV-2 proteins are targeted by immune molecules called antibodies, which help to fight infection.
The team found that 15 people with COVID-19 had more antibodies against 11 viral proteins than did healthy people before the pandemic (A. Hachim et al. Preprint at medRxiv http://doi.org/ggtrxh; 2020). Tests for antibodies against three of these proteins distinguished infected people from healthy controls.Much of the effort to develop vaccines and diagnostic tests has focused on a viral protein called Spike. But these results, which have not yet been peer-reviewed, suggest that other proteins might also be important determinants of immunity against SARS-CoV-2.
11 May — High risk of COVID-19 death for minority ethnic groups is a troubling mystery
People who are not white face a substantially higher risk of dying from COVID-19 than do white people — and pre-existing health conditions and socioeconomic factors explain only a small part of the higher risk.
In the most sweeping study of its kind, Ben Goldacre at the University of Oxford, UK, and his colleagues examined the medical records of more than 17 million residents of England (E. Williamson et al. Preprint at medRxiv http://doi.org/dt9z; 2020). The analysis, which has not yet been peer reviewed, showed that medical conditions such as diabetes are linked to a higher risk of death from the new coronavirus.
But the prevalence of such conditions in people who belong to minority ethnic groups plays only a small part in the heightened risk, as does the prevalence of social disadvantages such as low income. The researchers say that there is an urgent need for better measures to protect people in minority ethnic groups from the disease.
8 May — A strong antibody response is common in people who’ve recovered
Nearly everyone who recovers from COVID-19 makes antibodies against the new coronavirus, according to a study of more than 1,300 people who had symptoms of the disease.
Ania Wajnberg, Carlos Cordon-Cardo and their colleagues at the Icahn School of Medicine at Mount Sinai in New York City found that more than 99% of study participants who had been infected eventually developed antibodies — suggesting that they are immune from reinfection for an unknown length of time (A. Wajnberg et al. Preprint at medRxiv http://doi.org/dt5t; 2020). The immune response could be slow: some study volunteers didn’t produce detectable antibodies until one month after they first started feeling ill. The team found that a person’s age and sex didn’t affect their chance of developing antibodies.
Almost 20% of study volunteers tested positive for viral RNA two or more weeks after their symptoms ended. This might mean that the presence of viral RNA is not a good indicator of whether the body has cleared the virus. The study has not yet been peer reviewed.
7 May — Even laypeople could use this new test to detect the coronavirus
A test that uses a CRISPR gene-editing system can detect the new coronavirus in an hour, without the need for specialized equipment or trained personnel.
Feng Zhang at the Broad Institute of MIT and Harvard in Cambridge, Massachusetts, and his colleagues sought to develop a test for SARS-CoV-2 that would be quicker and simpler than the current procedure, which requires expensive lab equipment and scarce reagents. The team’s CRISPR-based protocol can be performed by a layperson with access to a sous vide cooker, a piece of kitchen equipment that is commonly available for less than US$40 (J. Joung et al. Preprint at https://go.nature.com/35csgqk; 2020). The test makes results available on paper strips similar to those used in pregnancy tests. The results have not yet been peer reviewed.
The team says the test could be used in doctors’ offices, workplaces and other settings where fast diagnosis is necessary.
6 May — Speedy technique churns out synthetic viruses
Researchers have used yeast cells to create a synthetic version of the SARS-CoV-2 genome much more quickly than other methods can achieve.
The SARS-CoV-2 genome is composed of RNA, but the protocol developed by Joerg Jores and Volker Thiel at the University of Bern in Switzerland and their colleagues uses a dozen overlapping stretches of the SARS-CoV-2 genome converted into DNA (T. T. N. Thao et al. Nature http://doi.org/ggttcr; 2020). The team inserted these DNA fragments into cells of the yeast Saccharomyces cerevisiae, which stitched them into a complete viral genome.
The team then built live viruses by converting the synthetic genome back into RNA and inserting these strands into human cells. The synthetic coronaviruses took a week to make. The technique could be used to assemble viruses rapidly to study the biological effects of new mutations, the researchers say.
5 May — What stopped the epidemic in China? Two teams show there is no easy answer
New evidence shows the value of school closures, travel bans and other painful measures in curbing the coronavirus epidemic in China.
Marco Ajelli at the Bruno Kessler Foundation in Trento, Italy, Hongjie Yu at Fudan University in Shanghai and their colleagues found that after authorities mandated a stringent lockdown, people in Shanghai and Wuhan cut their encounters with others from 15–20 per day to roughly 2 per day (J. Zhang et al. Science http://doi.org/ggthtr; 2020). This drastic social distancing was enough to bring the epidemic under control in the two cities.
The team’s modelling work suggests that, in Shanghai, school closures alone would not have stopped the epidemic — but did lower the number of new infections per day at the epidemic’s peak, which relieved stress on hospitals.
Another study, by Shengjie Lai at the University of Southampton, UK, and his colleagues, shows that quick detection of infections and isolation of infected people were the most effective steps for containing COVID-19 cases in China (S. Lai et al. Nature http://doi.org/dtr4; 2020). But even with those efforts in place, the number of cases would have soared if officials hadn’t restricted travel and social interactions, as well.
If epidemic-control actions had been delayed by only three weeks, the number of infected people in China might have been 18 times higher, the authors found.
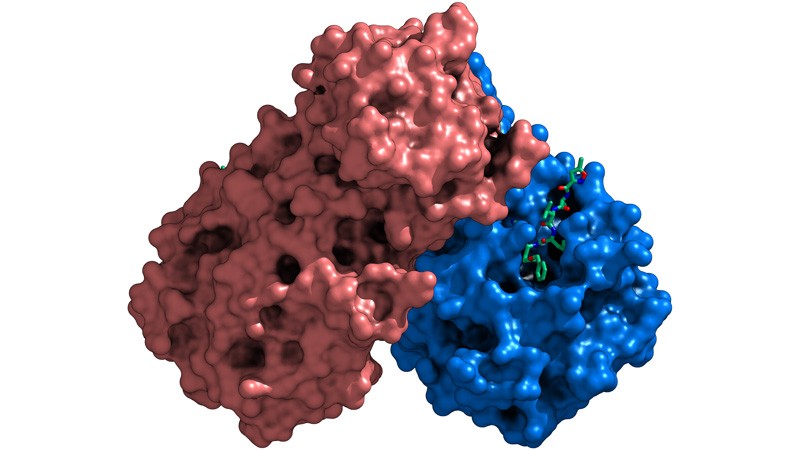
4 May — Portraits of a viral enzyme could aid hunt for drugs
Molecular snapshots of a key SARS-CoV-2 enzyme in action provide clues to how drugs, including the experimental therapy remdesivir, attack the virus.
Remdesivir has been shown in an early trial to speed up the recovery of people with COVID-19. The compound blocks the action of a viral enzyme called an RNA-dependent RNA polymerase.
A team led by Patrick Cramer at the Max Planck Institute for Biophysical Chemistry in Göttingen, Germany, used an imaging technique called cryo-electron microscopy to map the 3D shape of the enzyme as it copied the virus’s genetic material (H. S. Hillen et al. Preprint at bioRxiv http://doi.org/dtgw; 2020; not peer reviewed before posting). The researchers say that further studies of the polymerase could lead to the identification of new antiviral compounds.
A separate team led by Eric Xu at the Shanghai Institute of Materia Medica in China solved the structure of the polymerase while it was linked to an RNA snippet incorporating a molecule of remdesivir (W. Yin et al. Science http://doi.org/dtnb; 2020). The results could help researchers to design powerful drugs that block the polymerase’s activity, the authors say.
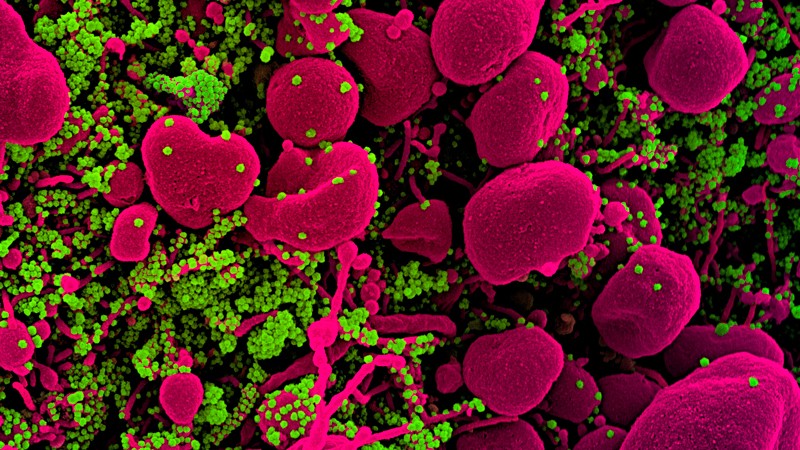
1 May — Immune system shows abnormal response to COVID-19
The immune response to SARS-CoV-2 differs from the response prompted by other respiratory viruses, according to an analysis of infected cells, ferrets and people. The finding supports the idea that treatments targeting the immune system could help people with COVID-19.
Benjamin tenOever at the Icahn School of Medicine at Mount Sinai in New York City and his colleagues found that cells infected with SARS-CoV-2 produce unusually low levels of antiviral proteins called interferons compared with cells infected with other respiratory viruses (D. Blanco-Melo et al. Cell https://go.nature.com/3bWE82b, 2020). But levels of some proteins, such as IL-6, that activate more general immune responses are higher in infected ferrets and people than in uninfected controls.
The results suggest an immune imbalance: low levels of interferons reduce a cell’s ability to limit viral replication, and the activation of less-specific immune responses promotes inflammation.
30 April — Young children are not immune to COVID-19
Children are as likely as adults to become infected with SARS-CoV-2 after close contact with an infected person, according to a study of people in Shenzhen, China.
Justin Lessler at Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland, Tiejian Feng at the Shenzhen Center for Disease Control and Prevention and their colleagues analysed nearly 400 cases of COVID-19 and 1,300 people who were ‘close contacts’ of the infected people (Q. Bi et al. Lancet Inf. Dis. http://doi.org/dtd7; 2020). The team found that 7% of close contacts younger than age 10 became infected — roughly the same as in the population overall. The work was first posted online as a preprint 27 March (http://doi.org/dpf9).
The researchers also found that just 9% of original cases were responsible for 80% of infections detected in close contacts. Such ‘superspreading’ events could lead to “large COVID-19 clusters”, the authors write.
29 April — SARS-CoV-2 might invade by hijacking its host’s immune defences
The new coronavirus invades human cells after one of its proteins binds with ACE2, a protein found in cells in many human organs. But little has been known about that crucial interaction.
To learn more, Alex Shalek at Harvard Medical School and the Massachusetts Institute of Technology (MIT) in Boston, Jose Ordovas-Montanes at the Broad Institute of MIT and Harvard in Cambridge, Massachusetts, and their colleagues studied airway cells from people with influenza (C. G. K. Ziegler et al. Cell http://doi.org/ds9j ; 2020). Both influenza virus and SARS-CoV-2 invade the respiratory tract.
The team found that in people with flu, signalling molecules called interferons — which normally help to fend off viruses — switch on the host genes encoding the ACE2 protein. The result suggests that the body’s defences against viral attack drive the activation of the gene for ACE2.
28 April — ‘Dry swabbing’ offers a workaround to test-chemical scarcity
Wide-scale genetic testing for SARS-CoV-2 has been hampered, in part, by shortages of the solutions used to store sampling swabs and extract viral RNA from them. To overcome this difficulty, a team led by Lea Starita and Jay Shendure at the University of Washington in Seattle developed a procedure for detecting viral RNA in swabs without the highly sought solutions (S. Srivatsan et al. Preprint at bioRxiv http://doi.org/ds6k; 2020; not peer reviewed before posting).
The ‘dry swab, extraction-free’ procedure correctly detected viral RNA in 9 out of 11 samples from people known to have SARS-CoV-2 infections. Conventional extraction methods yielded positive results in only 8 of the 11. The researchers say that their protocol could enable a massive scale-up in the use of self-collected samples for genetic testing at centralized laboratories.
27 April — Hospital toilets can be a hotspot for airborne viral RNA
The new coronavirus’s RNA can travel through the air, and might spread by way of small particles exhaled by infected people.
Ke Lan at Wuhan University in China and his colleagues tested the concentration of SARS-CoV-2 RNA in aerosols — fine airborne particles — at two hospitals treating people with COVID-19 (Y. Liu et al. Nature https://doi.org/10.1038/s41586-020-2271-3; 2020).
The team detected elevated levels of viral RNA in locations such as a small toilet used by patients, and staff changing rooms. No viral RNA was detected in staff rooms after they had been disinfected. Low to undetectable levels were found in the hospitals’ well-ventilated patient wards.
The presence of airborne viral RNA suggests that SARS-CoV-2 has the potential to spread by way of aerosols, the researchers say. They suggest that measures such as routine disinfection and better ventilation could help to control the virus’s spread.
24 April — Spit could be the solution to testing shortages
A person’s saliva accurately reveals whether they are infected with SARS-CoV-2, a finding that could make tests for the virus safer and more widely available.
The gold-standard test for coronavirus infection requires a long swab to be rubbed against the back of the throat. But such swabs are in short supply, and swabbing can prompt people to cough or sneeze, potentially launching a barrage of viral particles.
Anne Wyllie at the Yale School of Public Health in New Haven, Connecticut, and her colleagues collected both saliva and throat samples from people hospitalized with COVID-19 (A. Wyllie et al. Preprint at medRxiv, http://doi.org/ggssqf, 2020; not peer reviewed before posting). The team’s testing did not detect the virus in some patients’ throat-swab samples — but did detect it in the same patients’ saliva samples. Saliva testing also showed that two health-care workers who felt fine and had negative throat tests were actually infected.
23 April — Intensive testing finds a small town’s many silent infections
A large proportion of people with COVID-19 have no symptoms, according to research in a small Italian town.
On 21 February, the town of Vo’ reported Italy’s first COVID-19 death, leading authorities to ban movement in the town and end public services and commercial activities there for two weeks. Andrea Crisanti at Imperial College London and his colleagues swabbed almost every resident of Vo’ for viral RNA at the beginning and end of the lockdown.
The team found that some 43% of the people infected with SARS-CoV-2 in the town reported no fever or other symptoms (E. Lavezzo et al. Preprint at medRxiv http://doi.org/ggsmcj; 2020; not peer reviewed before posting). The researchers observed no statistically significant difference in potential infectiousness between those who reported symptoms and those who did not.
Asymptomatic and pre-symptomatic individuals have a key role in COVID-19 transmission, which makes it difficult to control the disease without strict social distancing, the authors say.
22 April — A vaccine candidate shows early success in an animal trial
An experimental vaccine protects monkeys from infection with the virus that causes COVID-19.
A team led by Chuan Qin at the Peking Union Medical College in Beijing injected rhesus macaques (Macaca mulatta) with three doses of a vaccine comprised of chemically inactivated particles of SARS-CoV-2 (Q. Gao et al. Preprint at bioRxiv http://doi.org/dskt; 2020; not peer reviewed before posting). Eight monkeys were then intentionally exposed to the virus.
All four monkeys given a high dose of the vaccine had no detectable virus in their throat or lungs seven days after exposure. Monkeys that received a lower dose of vaccine showed some signs of coronavirus infection — but their levels of virus were much lower than in exposed animals that received no vaccine. This month, the company developing the vaccine received approval to start human safety trials on it.
20 April — How Hong Kong stemmed viral spread without harsh restrictions
Hong Kong slowed the spread of SARS-CoV-2 through a combination of intensive surveillance, quarantining and social distancing without relying on severe measures used elsewhere.
In January, the authorities in Wuhan, where the coronavirus outbreak began, halted travel out of the city in an attempt to control the spread of the virus that causes COVID-19. But Hong Kong relied on a programme that included widespread testing, quarantining of those who had been in contact with infected people, and distancing measures such as school closures. When Peng Wu at the University of Hong Kong and her colleagues surveyed residents in early March, 99% said they wore a mask in public and 85% said they avoided crowds (B. J. Cowling et al. Lancet Public Health http://doi.org/dsfw; 2020).
The combination of public behavioural changes and government measures kept the virus’s spread relatively low in Hong Kong during the period to the end of March, the team found.
17 April — Vaccine from viral spikes holds promise
A key portion of a coronavirus protein could form the basis of a safe and effective vaccine.
Coronavirus particles bristle with spiny ‘spike proteins’. A portion of the spike called the receptor-binding domain recognizes and attaches to a molecule found on the surface of many human cells, allowing the viral particle to gain entry into those cells.
Hyeryun Choe and Michael Farzan at the Scripps Research Institute in Jupiter, Florida, and their colleagues immunized rats with fragments of the spike’s binding domain (B. D. Quinlan et al. Preprint at bioRxiv, http://doi.org/ggrs5t; 2020; not peer reviewed before posting). In response, the rodents’ immune systems made antibodies that can recognize coronavirus and prevent it from infecting cells.
Further experiments suggested that these antibodies are unlikely to make host cells more susceptible to coronavirus infection — one of the main safety concerns for vaccines.
16 April — Ski buffs helped to seed coronavirus in Iceland
Holidaymakers returning from ski trips to the Alps helped to bring the coronavirus to Iceland.
In late January, Kari Stefansson at deCODE Genetics-Amgen in Reykjavik and his colleagues began testing for SARS-CoV-2 among Iceland residents at high risk of exposure to the virus, such as travellers to China (D. F. Gudbjartsson et al. N. Engl. J. Med. http://doi.org/ggr6wx; 2020). Some 13% of the 9,199 people tested by early April were infected. The team sequenced viral RNA from people who tested positive and found that some of the strains had probably originated in Austria or Italy, which both have Alpine ski resorts.
Tests in the second half of March on more than 2,000 randomly selected individuals found that only 0.6% were infected. The researchers say their analysis suggests that measures to contain the virus through testing, contact tracing and quarantining have been successful in Iceland.
15 April — Relief from social distancing could unleash the virus anew
Cases of COVID-19 are likely to surge after current social-distancing measures are eased, according to models.
Yonatan Grad, Marc Lipsitch and their colleagues at the Harvard T.H. Chan School of Public Health in Boston, Massachusetts, modelled the spread of coronaviruses in places that have temperate climates, such as the United States. The results helped the team to predict the spread of SARS-CoV-2, the coronavirus that causes COVID-19 (S.M. Kissler et al. Science http://doi.org/drz3; 2020).
The researchers found that if SARS-CoV-2 spreads more efficiently in some seasons than in others — as influenza virus does, for example — the peak number of COVID-19 cases after social distancing ends could be larger than the peak number without any social distancing at all. That’s because distancing measures leave a high proportion of people susceptible to infection, leading to a spike of disease if viral transmission ramps up late in the year.
If human immunity to SARS-CoV-2 wanes over the course of a few years, the virus is likely to cause repeated outbreaks in wintertime, the authors say.
15 April — Common sequencing technique could speed large-scale diagnosis
A standard genomic-analysis method that can sequence tens of thousands of DNA samples in a day has been adapted to detect the virus that causes COVID-19.
In a testing protocol proposed by Jonathan Schmid-Burgk at the Broad Institute of MIT and Harvard in Cambridge, Massachusetts, and his team, every sample being tested for SARS-CoV-2 would be tagged with a unique DNA sequence that would serve as a biological barcode (J. L. Schmid-Burgk et al. Preprint at bioRxiv, http://doi.org/drzc; 2020; not peer reviewed before posting). High-speed sequencing instruments common in research laboratories around the world could then be used to analyse as many as 100,000 DNA samples at one time.
The authors anticipate that if clinical testing validates the method, then millions of samples could be analysed per day at each sequencing site — a far more efficient output than that of current testing techniques.
Correction: An earlier version did not include the name of the paper’s corresponding author, Jonathan Schmid-Burgk.
10 April — A viral enzyme’s structure points to possible drugs
Scientists have detailed the crystal structure of one of SARS-CoV-2’s key proteins, an enzyme called a protease that the virus needs to replicate within our cells.
Hualiang Jiang, Zihe Rao and Haitao Yang at ShanghaiTech University in China and their colleagues deposited the structure in a protein data bank two months ago, and have since used it to help them identify compounds that inhibit the protease (Z. Jin et al. Nature https://doi.org/10.1038/s41586-020-2223-y; 2020). The team’s screening revealed several powerful viral inhibitors, including ebselen, whose safety has already been tested in people.
These inhibitors work by infiltrating a hollow in the protease. Proteases found in other coronaviruses have a similar hollow, raising hopes that a single compound might help to treat a wide variety of diseases caused by coronaviruses.
9 April — Absent antibodies suggest mystery immune response
After recovering from infection with SARS-Cov-2, many people have high levels of antibodies against the virus. But a recent study finds that in some recovered patients, such antibodies are present at very low levels — and in some cases are undetectable.
When a foreign microbe intrudes on the body, the immune system usually makes proteins called antibodies that help to fight off the invader. A team led by Jinghe Huang and Fan Wu at Fudan University in Shanghai, China measured antibodies to the novel coronavirus in 175 volunteers who had recovered from mild infections (F. Wu et al. https://www.medrxiv.org/content/10.1101/2020.03.30.20047365v1, 2020; not peer reviewed before posting). About 30% of the volunteers — and especially those under the age of 40 — never developed high levels of SARS-CoV-2 antibodies, suggesting that other immune responses helped rid them of their infections.
8 April — Viral load soars as infected people start feeling ill
Viral RNA levels are highest in people with COVID-19 soon after their symptoms appear, according to two separate research teams.
Kwok-Yung Yuen at The University of Hong Kong–Shenzhen Hospital, China, and his colleagues analysed saliva samples coughed up by 23 people infected with SARS-CoV-2. The team found that study participants’ viral concentrations peaked shortly after they started feeling ill, and began declining about one week after the peak.
The more viral RNA detected in a person’s body, the more they excrete when coughing or sneezing. The authors say that the high levels of SARS-CoV-2 particles detected at the onset of symptoms suggest that the virus can be transmitted easily between people, even when symptoms are relatively mild (K. K.-W. To et al. Lancet Infect. Dis. http://doi.org/ggp4qx; 2020).
The results are consistent with another study of nose and throat swabs from 18 people with COVID-19. The concentrations of viral RNA in the 17 symptomatic patients were similar to that in the one asymptomatic patient (L. Zou et al. N. Engl. J. Med. http://doi.org/ggmzsp; 2020).
However, another study found that people with milder COVID-19 symptoms on admission to hospital had much lower concentrations of viral RNA than did those with more severe symptoms (Y. Liu et al. Lancet Infect. Dis. http://doi.org/dqrr; 2020). Wei Zhang at The First Affiliated Hospital of Nanchang University, China, Leo Poon at the University of Hong Kong, and their colleagues say the findings suggest that viral RNA concentrations could predict whether infected people will develop more severe symptoms.
7 April — A comparison finds subtle differences between tests for the COVID-19 virus
Doctors rely on a test called quantitative reverse-transcription polymerase chain reaction (qRT-PCR) to determine whether a person is infected with SARS-CoV-2. A team led by Nathan Grubaugh at Yale School of Public Health in New Haven, Connecticut, compared nine widely used versions of the test and found that all of them reliably detect the virus (C. B. F. Vogels et al. Preprint at medRxiv https://www.medrxiv.org/content/10.1101/2020.03.30.20048108v1; 2020; not peer reviewed before posting).
But the researchers also found that some tests — including one made by the US Centers for Disease Control and Prevention, another developed at Hong Kong University, and a third from Charité–Universitätsmedizin Berlin — performed best when it came to detecting low levels of the virus in samples.
5 April — Bats harbour a pool of coronaviruses related to pandemic culprit
Viruses closely related to SARS-CoV-2, the virus causing the COVID-19 pandemic, have been circulating in horseshoe bats, ready to jump to humans, for decades — and maybe even longer.
David Robertson at the University of Glasgow, UK, and his colleagues analysed the RNA of 68 coronaviruses, including SARS-CoV-2 and the virus that causes severe acute respiratory syndrome, or SARS (M. F. Boni et al. Preprint at bioRxiv https://doi.org/10.1101/2020.03.30.015008; 2020; not peer reviewed before posting). This analysis shows that horseshoe bats (Rhinolophus spp.) host an expanding lineage of viruses that, like SARS-CoV-2, can infect humans. The team estimates that the ancestor of SARS-CoV-2 split 40 to 70 years ago from the closely related bat virus RaTG13. Though the two viruses are highly similar genetically, RaTG13 doesn’t infect humans.
The analysis also suggests that viruses in the lineage are ready to jump to humans directly from bats. But SARS-CoV-2 might have first hopped to another species that humans are more exposed to, rather than spreading straight from bat to human.
3 April — Masks could cut spread of COVID-19 virus
Surgical face masks effectively block the spread of seasonal coronaviruses in respiratory droplets, suggesting that masks could prevent transmission of SARS-CoV-2.
Seasonal coronaviruses are one cause of the common cold. Benjamin Cowling at the University of Hong Kong and his colleagues had ill volunteers who were infected with seasonal coronaviruses sit in an enclosed booth and place their faces in a sampling device, called the Gesundheit-II, that captures airborne particles (N. H. L. Leung et al. Nat. Med. https://doi.org/10.1038/s41591-020-0843-2; 2020).
The scientists detected coronavirus RNA in both coarse droplets and finer ‘aerosol’ droplets emitted by volunteers who were not wearing masks. Mask reduced detection of viral RNA in both types of droplet. Larger particles are carried by sneezes and coughs, whereas exhaled breath can spread aerosol droplets, which have a diameter of five micrometres or less.
The authors say that surgical masks reduce transmission of not only seasonal coronaviruses, but also influenza.
Correction: An earlier version of this article said masks reduced detection of viral DNA.
1 April — Antibodies from llamas help to foil the COVID-19 virus
Antibodies from llamas (Lama glama) could help in the fight against several coronaviruses that infect humans.
A team led by Bert Schepens and Xavier Saelens of the VIB life-sciences institute in Ghent, Belgium, and Jason McLellan of the University of Texas at Austin has isolated two llama antibodies that bind the ‘spike’ proteins that coronaviruses use to enter cells (D. Wrapp et al. Preprint at bioRxiv https://doi.org/10.1101/2020.03.26.010165; 2020; not peer reviewed before posting). One antibody neutralized the coronavirus responsible for Middle East respiratory syndrome (MERS); the second mopped up the severe acute respiratory syndrome (SARS) coronavirus.
Fusing the SARS antibody from a llama with an antibody from a human yielded a hybrid that neutralized the virus responsible for COVID-19. The data suggest that such antibodies could be useful in combating coronavirus epidemics
30 March — Debilitated patients rally after dose of survivors’ blood
People seriously ill with COVID-19 experienced striking improvement after receiving infusions of blood from disease survivors, according to two separate research teams.
Both teams extracted antibody-laden plasma — a component of blood — from people who’d recovered from COVID-19.
Xiaoming Yang at the National Engineering Technology Research Center for Combined Vaccines in Wuhan, China, and his colleagues gave the plasma to ten severely ill people. By the sixth day after the treatment, the virus that causes COVID-19 was undetectable in seven of the ten. The recipients experienced no significant side effects (K. Duan et al. Preprint at medRxiv http://doi.org/dqrs; 2020; not peer reviewed before posting).
A group led by Lei Liu at Shenzhen Third People’s Hospital in China gave survivors’ plasma to five “critically ill” people (C. Shen et al. J. Am. Med. Assoc. http://doi.org/dqn7; 2020). Symptoms dwindled in all five; within ten days of receiving the plasma, three recipients no longer needed ventilators.
Other researchers would like to try such transfusions to treat health workers who have been directly exposed.
27 March — Viral proteins point to potential treatments
A list of the human proteins affected by the SARS-CoV-2 virus offers a guide to potential treatments for infected people.
A team led by Nevan Krogan at the University of California, San Francisco, engineered human cells to produce one of 26 proteins made by the coronavirus (D. E. Gordon et al. Preprint at bioRxiv https://doi.org/10.1101/2020.03.22.002386; 2020; not peer reviewed before posting). This allowed the researchers to identify human proteins that physically interact with coronavirus proteins.
Out of 332 interactions between human and viral proteins, the authors identified 67 that existing or candidate drugs could potentially disrupt. The researchers and their collaborators are now testing some of these compounds for antiviral activity — and urge others to do the same.
https://www.nature.com/articles/d41586-020-00502-w






















No hay comentarios:
Publicar un comentario