Interferon Resistance of Emerging SARS-CoV-2 Variants
Kejun Guo, Bradley S. Barrett, Kaylee L. Mickens, Kim J. Hasenkrug, View ORCID ProfileMario L. Santiago
Abstract
La aparición de variantes del SARS-CoV-2 con mayor transmisibilidad, patogénesis y resistencia a las vacunas plantea retos urgentes para frenar la pandemia de COVID-19. Mientras que las mutaciones de Spike que mejoran la infectividad del virus pueden impulsar la aparición de estas nuevas variantes, los estudios que documentan un papel crítico de las respuestas de los interferones en el control temprano de la infección por SARS-CoV-2, junto con la presencia de genes virales que limitan estas respuestas, sugieren que los interferones también pueden influir en la evolución del SARS-CoV-2. Aquí, comparamos la potencia de 17 interferones humanos diferentes contra 5 linajes virales muestreados durante el curso del brote global que incluía variantes ancestrales y emergentes. Nuestros datos revelaron una mayor resistencia al interferón en las variantes emergentes del SARS-CoV-2, lo que indica que la evasión de la inmunidad innata es una fuerza motriz importante para la evolución del SARS-CoV-2. Estos hallazgos tienen implicaciones en el aumento de la letalidad de las variantes emergentes y ponen de relieve los subtipos de interferón que pueden tener más éxito en el tratamiento de las primeras infecciones.
El genoma humano codifica una amplia gama de interferones (IFN) antivirales. Entre ellos se encuentran los IFN de tipo I (IFN-I), como los 12 subtipos de IFNα, IFNβ e IFNω, que señalan a través del receptor IFNAR ubicuo, y los IFN de tipo III (IFN-III), como IFNλ1, IFNλ2 e IFNλ3, que señalan a través del receptor IFNλR, más restringido, que está presente en las células epiteliales pulmonares1. La diversidad de IFN puede estar impulsada por una carrera armamentística evolutiva para permitir al huésped contrarrestar diversos patógenos virales2. Por ejemplo, los subtipos de IFNα presentan una identidad de secuencia de aminoácidos superior al 78%, pero el IFNα14, el IFNα8 y el IFNα6 son los más potentes para inhibir el VIH-1 in vitro e in vivo3-5, mientras que el IFNα5 es el más potente para inhibir la gripe H3N2 en cultivos de explantes pulmonares6. Sorprendentemente, aunque el SARS-CoV-2 fue sensible al IFNα2, el IFNβ y el IFNλ7-9, y los ensayos clínicos sobre el IFNα2 y el IFNβ demostraron resultados prometedores contra el COVID-1910-12, todavía no se ha realizado una comparación directa de múltiples IFN-I y IFN-III contra diversos aislados de SARS-CoV-2.
Results
The
current study was undertaken to determine which IFNs would best inhibit
SARS-CoV-2. We selected 5 isolates from prominent lineages13 during the course of the pandemic (Fig. 1, Supplementary Table 1). USA-WA1/2020 is the standard strain utilized in many in vitro and in vivo studies of SARS-CoV-2 and belongs to lineage A13.
It was isolated from the first COVID-19 patient in the US, who had a
direct epidemiologic link to Wuhan, China, where the virus was first
detected14. By contrast, subsequent infection waves from Asia to Europe15 were associated with the emergence of the D614G mutation16. D614G+ strains in lineage B spread with devastating speed, likely due to its increased transmissibility17,18. It accumulated additional mutations in Italy as lineage B.1 which then precipitated a severe outbreak in New York City19.
More recently, lineage B.1.1.7 acquired the N501Y mutation that is
associated with enhanced transmissibility in the United Kingdom13.
Lineage B.1.351 was first reported in South Africa and acquired an
additional E484K mutation that is associated with resistance to
neutralizing antibodies20,21.
Both B.1.1.7 and B.1.351 have now been reported in multiple countries
and there is increasing concern that these may become dominant22.
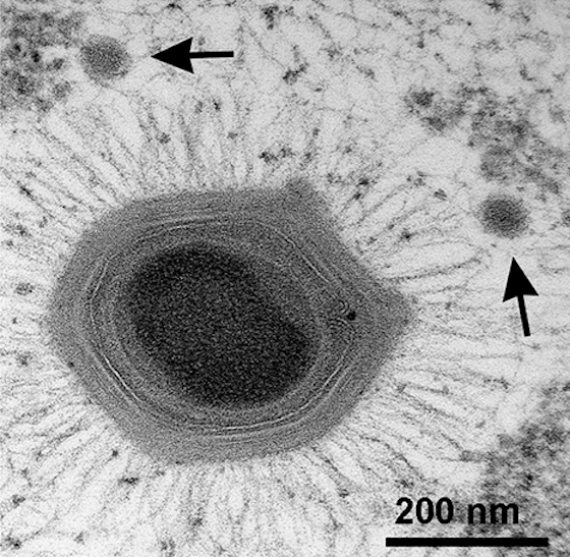
Representative SARS-CoV-2 isolates from the B, B.1, B.1.1.7 and B.1.351
lineages were obtained from BEI Resources (Supplementary Table 1) and
amplified once in an alveolar type II epithelial cell line, A549, that
we stably transduced with the receptor ACE2 (A549-ACE2) (Supplementary
Fig. 1a).
A549-ACE2
cells were pre-incubated with 17 recombinant IFNs (PBL Assay Science)
overnight in parallel and in triplicate, then infected with a
non-saturating virus dose for 2 h (Supplementary Fig. 1b). We normalized
the IFNs based on molar concentrations similar to our previous work
with HIV-13,23.
For rapid and robust evaluation of antiviral activities against live
SARS-CoV-2 isolates, we utilized a quantitative PCR approach (Fig. 2a).
An initial dose-titration study showed that a 2 pM concentration
maximally distinguished the antiviral activities of IFNβ and IFNλ1
(Supplementary Fig. 1c), and was therefore used to screen the antiviral
IFNs. In the absence of IFN, all 5 isolates reached titers of ~104-106 copies per 5 μl input of RNA extract (Fig. 2). Using absolute copy numbers (Fig. 2)
and values normalized to mock as 100% (Supplementary Fig. 2), the 17
IFNs showed a range of antiviral activities against SARS-CoV-2. The 3
IFNλ subtypes exhibited none to very weak (<2-fold) antiviral
activities compared to most IFN-Is (Fig. 2
and Supplementary Fig. 2, blue bars). This was despite the fact that
the assay showed a robust dynamic range, with some IFNs inhibiting
USA-WA1/2020 >2500-fold to below detectable levels (Fig. 2a).
IFN potencies against the 5 isolates correlated with each other
(Supplementary Fig. 3), and a similar rank-order of IFN antiviral
potency was observed for D614G+ isolates (Fig. 2b, Supplementary Fig. 2). Overall, IFNα8, IFNβ and IFNω were the most potent, followed by IFNα5, IFNα17 and IFNα14 (Fig. 2c).
We
reported that HIV-1 inhibition by the IFNα subtypes correlated with
IFNAR signaling capacity and binding affinity to the IFNAR2 subunit3,23.
IFNAR signaling capacity, as measured in an IFN-sensitive reporter cell
line (iLite cells; Euro Diagnostics), correlated with the antiviral
potencies of the IFNα subtypes against SARS-CoV-2 lineages A and B, but
not B.1, B.1.351 or B.1.1.7 strains (Fig. 3a). Interestingly, IFNα subtype inhibition of SARS-CoV-2 did not correlate with IFNAR2 binding affinity (Fig. 3b)24, as measured by surface plasmon resonance by the Schreiber group24. Furthermore, correlations between SARS-CoV-2 and HIV-1 inhibition3 were weak at best (Fig. 3c). These findings suggested that IFN-mediated control of SARS-CoV-2 isolates may be qualitatively distinct from that of HIV-1.
We
generated a heat-map to visualize the antiviral potency of diverse IFNs
against the 5 isolates and observed marked differences in IFN
sensitivities (Fig. 4a).
Pairwise analysis of antiviral potencies between isolates collected
early (January 2020) and later (March-December 2020) during the pandemic
were performed against the 14 IFN-Is (IFN-IIIs were not included due to
low inhibition, Fig. 2).
The overall IFN-I sensitivity of USA-WA1/2020 and Germany/BavPat1/2020
isolates were not significantly different from each other (Fig. 4b).
By contrast, relative to Germany/BavPat1/2020, we observed 17 to
122-fold IFN-I resistance of the emerging SARS-CoV-2 variants (Fig. 4c),
with the B.1.1.7 strain exhibiting the highest IFN-I resistance. The
level of interferon resistance was more striking when compared to
USA-WA1/2020, where emerging SARS-CoV-2 variants exhibited 25 to
322-fold higher IFN-I resistance (Supplementary Fig. 4a).
The
experiments above allowed the simultaneous analysis of 17 IFNs against
multiple SARS-CoV-2 isolates, but do not provide information on how
different IFN-I doses affect virus replication. It also remains unclear
if the emerging variants were resistant to IFN-IIIs. We therefore
titrated a potent (IFNβ; 0.002 to 200 pM) and a weak (IFNλ1; 0.02 to
2000 pM) interferon against the lineage B, B.1, B.1.1.7 and B.1.351
isolates (Fig. 4d
and Supplementary Fig. 4b). We included an additional B.1.1.7 strain,
hCov-19/England/204820464/2020 (Supplementary Table 1). The 50%
inhibitory concentrations (IC50) of the B.1.1.7 variants were 4.3 to 8.3-fold higher for IFNβ and 3.0 to 3.5 higher for IFNλ1 than the lineage B isolate (Fig. 4d), whereas the B.1 isolate exhibited 2.6 and 5.5-fold higher IC50
for IFNλ1 and IFNβ, respectively (Supplementary Fig. 4b).
Interestingly, maximum inhibition was not achieved with either IFNβ or
IFNλ1 against the B.1.1.7 variant, plateauing at 15 to 20-fold higher
levels than the ancestral lineage B isolate (Fig. 4d).
In a separate experiment, the B.1.351 variant was also more resistant
to IFNβ (>500-fold) and IFNλ1 (26-fold) compared to the lineage B
isolate (Fig. 4d). These data confirm that the B.1, B.1.1.7 and B.1.351 isolates have evolved to resist the IFN-I and IFN-III response.
Discussion
Numerosos estudios realizados por muchos laboratorios pusieron de manifiesto la importancia de los IFN en el control del SARS-CoV-2. Aquí demostramos la continua evolución del SARS-CoV-2 para escapar a las respuestas de los IFN e identificamos los IFN con las mayores potencias antivirales. El IFNλ se mostró inicialmente prometedor como antiviral que puede reducir la inflamación25, pero recientemente se asoció con la patología pulmonar inducida por el virus26. Nuestros datos sugieren que pueden ser necesarias dosis más altas de IFNλ para lograr un efecto antiviral in vivo similar al de los IFN-I. El IFNβ nebulizado mostró potencial como terapéutica contra el COVID-1911, y nuestros datos confirman que el IFNβ es un antiviral muy potente contra el SARS-CoV-2. Sin embargo, el IFNβ también se relacionó con resultados patogénicos en la infección crónica de la mucosa por el VIH-123, el LCMV27 murino y, si se administra tarde en ratones, el SARS-CoV-1 y el MERS-CoV28,29. Por el contrario, el IFNα8 alteró 3 veces menos genes en los linfocitos primarios de la mucosa que el IFNβ23, pero mostró una potencia anti-SARS-CoV-2 similar a la del IFNβ. El IFNα8 también mostró una elevada actividad antiviral contra el VIH-13, lo que aumenta su potencial para el tratamiento contra ambos virus pandémicos. En particular, el IFNα8 parecía ser un caso atípico, ya que las potencias antivirales de los subtipos de IFNα contra el SARS-CoV-2 y el VIH-1 no estaban fuertemente correlacionadas. El IFNα6 restringió potentemente el VIH-13,4 pero fue uno de los subtipos de IFNα más débiles contra el SARS-CoV-2. Por el contrario, el IFNα5 inhibió fuertemente el SARS-CoV-2, pero inhibió débilmente el VIH-13. Nuestros datos refuerzan la teoría de que los diversos IFN pueden haber evolucionado para restringir familias de virus distintas2,23. Los mecanismos subyacentes a estas diferencias cualitativas siguen sin estar claros. Mientras que la señalización del IFNAR contribuye a la potencia antiviral3,4,24, los diversos IFNs pueden tener distintas capacidades para movilizar efectores antivirales en tipos celulares específicos. La comparación de los interferomas inducidos por distintos IFN en las células epiteliales pulmonares puede ayudar a desentrañar los mecanismos antivirales responsables de los efectos diferenciales.
Our
data unmasked a concerning trend for emerging SARS-CoV-2 variants to
resist the antiviral IFN response. Prior to this work, the emergence and
fixation of variants was linked to enhanced viral infectivity due to
mutations in the Spike protein13,16–18. However, previous studies on HIV-1 infection suggested that IFNs can also shape the evolution of pandemic viruses30,31. In fact, SARS-CoV-2 infected individuals with either genetic defects in IFN signaling32 or IFN-reactive autoantibodies33
had increased risk of developing severe COVID-19. As IFNs are critical
in controlling early virus infection levels, IFN-resistant SARS-CoV-2
variants may produce higher viral loads that could in turn promote
transmission and/or exacerbate pathogenesis. Consistent with this
hypothesis, alarming preliminary reports linked B.1.1.7 with increased
viral loads34 and risk of death35–37.
In addition to Spike, emerging variants exhibited mutations in
nucleocapsid, membrane and nonstructural proteins NSP3, NSP6 and NSP12
(Supplementary Table 1). These viral proteins were shown to antagonize
IFN signaling in cells38–40.
It will be important to identify the virus mutations driving IFN-I
resistance in emerging variants, the underlying molecular mechanisms,
and its consequences for COVID-19 pathogenesis.
Overall,
the current study suggested a role for the innate immune response in
driving the evolution of SARS-CoV-2 that could have practical
implications for interferon-based therapies. Our findings reinforce the
importance of continued full-genome surveillance of SARS-CoV-2, and
assessments of emerging variants not only for resistance to
vaccine-elicited neutralizing antibodies, but also for evasion of the
host interferon response.
Materials and Methods
Cell lines
A549
cells were obtained from the American Type Culture Collection (ATCC)
and cultured in complete media containing F-12 Ham’s media (Corning),
10% fetal bovine serum (Atlanta Biologicals), 1%
penicillin/streptomycin/glutamine (Corning) and maintained at 37°C 5% CO2. A549 cells were transduced with codon-optimized human ACE2 (Genscript) cloned into pBABE-puro41 (Addgene). To generate the A549-ACE2 stable cell line, 107
HEK293T (ATCC) cells in T-175 flasks were transiently co-transfected
with 60 μg mixture of pBABE-puro-ACE2, pUMVC, and pCMV-VSV-G at a 10:9:1
ratio using a calcium phosphate method42. Forty-eight hours post transfection, the supernatant was collected, centrifuged at 1000×g
for 5 min and passed through a 0.45 μm syringe filter to remove cell
debris. The filtered virus was mixed with fresh media (30% vol/vol) that
included polybrene (Sigma) at a 6 μg/ml final concentration. The virus
mixture was added into 6-well plates with 5×105 A549
cells/well and media was changed once more after 12 h. Transduced cells
were selected in 0.5 μg/ml puromycin for 72 h, and ACE2 expression was
confirmed by flow cytometry, western blot and susceptibility to
HIV-1ΔEnv/SARS-CoV-2 Spike pseudovirions.
Virus isolates
All
experiments with live SARS-CoV-2 were performed in a Biosafety Level-3
(BSL3) facility with powered air-purifying respirators at the University
of Colorado Anschutz Medical Campus. SARS-CoV-2 stocks from BEI
Resources (Supplementary Table 1) had comparable titers >106 TCID50/ml
(Supplementary Fig. 1a) except for the B.1.1.7 strains
(CA_CDC_5574/2020 and England/204820464/2020). The contents of the
entire vial (~0.5 ml) were inoculated into 3 T-75 flasks containing 3×106
A549-ACE2 cells, except for B.1.1.7 which was inoculated into 1 T-75
flask. After culturing for 72 h, the supernatants were collected and
spun at 2700×g for 5 min to remove cell debris, and frozen at
−80°C. The A549-amplified stocks were titered according to the proposed
assay format (Supplementary Fig. 1b, Fig. 2a). Briefly, 2.5×;104
A549-ACE2 cells were plated per well in a 48-well plate overnight. The
next day, the cells were infected with 300, 30, 3, 0.3, 0.03 and 0.003
μl (serial 10-fold dilution) of amplified virus stock in 300 μl final
volume of media for 2 h. The virus was washed twice with PBS, and 500 μl
of complete media with the corresponding IFN concentrations were added.
After 24 h, supernatants were collected, and cell debris was removed by
centrifugation at 3200×g for 5 min.
SARS-CoV-2 quantitative PCR
For
rapid and robust assessments of viral replication, we utilized a
real-time quantitative PCR (qPCR) approach. This assay would require
less handling of infectious, potentially high-titer SARS-CoV-2 in the
BSL3 compared to a VeroE6 plaque assay, as the supernatants can be
directly placed in lysis buffer containing guanidinium thiocyanate that
would inactivate the virus by at least 4-5 log1043.
To measure SARS-CoV-2 levels, total RNA was extracted from 100 μl of
culture supernatant using the E.Z.N.A Total RNA Kit I (Omega Bio-Tek)
and eluted in 50 μl of RNAse-free water. 5 μl of this extract was used
for qPCR. Official CDC SARS-CoV-2 N1 primers and TaqMan probe set were
used44 with the Luna Universal Probe One-Step RT-qPCR Kit (New England Biolabs):
Forward primer: GACCCCAAAATCAGCGAAAT
Reverse primer: TCTGGTTACTGCCAGTTGAATCTG
TaqMan probe: FAM-ACCCCGCATTACGTTTGGTGGACC–TAMRA
The
sequence of the primers and probes were conserved against the 5
SARS-CoV-2 variants that were investigated. The real-time qPCR reaction
was run on a Bio-Rad CFX96 real-time thermocycler under the following
conditions: 55°C 10 mins for reverse transcription, then 95°C 1 min
followed by 40 cycles of 95°C 10s and 60°C 30s. The absolute
quantification of the N1 copy number was interpolated using a standard
curve with 107-101 serial 10-fold dilution of a control plasmid (nCoV-CDC-Control Plasmid, Eurofins).
Antiviral inhibition assay
We
used a non-saturating dose of the amplified virus stock for the IFN
inhibition assays. These titers were expected to yield ~105
copies per 5 μl input RNA extract (Supplementary Fig. 1b). Recombinant
IFNs were obtained from PBL Assay Science. In addition to the IFN-Is (12
IFNα subtypes, IFNβ and IFNω), we also evaluated 3 IFNλ subtypes
(IFNλ1, IFNλ2, IFNλ3). To normalize the IFNs, we used molar
concentrations23
instead of international units (IU), as IU values were derived from
inhibition of encelphalomyocarditis virus, which may not be relevant to
SARS-CoV-2. To find a suitable dose to screen 17 IFNs in parallel, we
performed a dose-titration experiment of the USA-WA1/2020 strain with
IFNβ and IFNλ1. A dose of 2 pM allowed for maximum discrimination of the
antiviral potency IFNβ versus IFNλ1 (Supplementary Fig. 1c). Serial
10-fold dilutions of IFNβ and IFNλ1 were also used in follow-up
experiments. Thus, in 48-well plates, we pre-incubated 2.5×104
A549-ACE2 cells with the IFNs for 18 h, then infected with the
A549-amplified virus stock for 2 h. After two washes with PBS, 500 μl
complete media containing the corresponding IFNs were added. The
cultures were incubated for another 24 h, after which, supernatants were
harvested for RNA extraction and qPCR analysis.
Statistical analyses
Data
were analyzed using GraphPad Prism 8. Differences between the IFNs were
tested using a nonparametric two-way analysis of variance (ANOVA)
followed by a multiple comparison using the Friedman test. Pearson
correlation coefficients (R2) values were computed for linear
regression analyses. Paired analysis of two isolates against multiple
IFNs were performed using a nonparametric, two-tailed Wilcoxon
matched-pairs rank test. Differences with p<0.05 were
considered significant. Nonlinear regression curves were fit using a
two-phase exponential decay equation on log-transformed data.
Acknowledgments
We
thank Cara Wilson, Ulf Dittmer and Kathrin Gibbert for scientific
advice; Mercedes Rincon and Elan Eisenmesser for assistance with
construction and characterization of the A549-ACE2 cells; Eric Poeschla,
James Morrison, Zach Wilson, Jill Garvey, Stephanie Torres-Nemeti and
Marcia Finucane for Biosafety Level-3 infrastructure support; and Roman
Wölfel, Rosina Ehmann, Adolfo García-Sastre, Alex Sigal, Tulio de
Oliveira, Bassam Hallis, the CDC and BEI Resources (NIAID) for the
SARS-CoV-2 isolates. This work was supported by the Department of
Medicine at the University of Colorado (MLS), NIH R01 AI134220 (MLS),
and the Intramural Research Program at the NIH, NIAID (KJH).
https://www.biorxiv.org/content/10.1101/2021.03.20.436257v1.full
https://notistecnicas.blogspot.com/2015/01/hepatitis-c-raymond-schinazzifarmacos.html
https://notistecnicas.blogspot.com/2020/03/murcielagos-vs-interferon-medicacion.html
https://notistecnicas.blogspot.com/2020/03/en-estudio-relacion-interferon-con.html
https://notistecnicas.blogspot.com/2020/05/la-combinacion-de-tres-antivirales.html
https://notistecnicas.blogspot.com/2020/05/fibrosis-pulmonar-y-covid.html
https://notistecnicas.blogspot.com/2015/01/hepatitis-c-raymond-schinazzifarmacos.html
https://notistecnicas.blogspot.com/2020/12/la-rapidez-en-encontrar-una.html
https://notistecnicas.blogspot.com/2020/03/bioestadistica-econometria-graficas.html