Annual Review of Microbiology
Vol. 73:529-557 (Volume publication date September 2019)
First published as a Review in Advance on June 21, 2019
https://doi.org/10.1146/annurev-micro-020518-115759
Abstract
Human
coronavirus (HCoV) infection causes respiratory diseases with mild to
severe outcomes. In the last 15 years, we have witnessed the emergence
of two zoonotic, highly pathogenic HCoVs: severe acute respiratory
syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome
coronavirus (MERS-CoV). Replication of HCoV is regulated by a diversity
of host factors and induces drastic alterations in cellular structure
and physiology. Activation of critical signaling pathways during HCoV
infection modulates the induction of antiviral immune response and
contributes to the pathogenesis of HCoV. Recent studies have begun to
reveal some fundamental aspects of the intricate HCoV-host interaction
in mechanistic detail. In this review, we summarize the current
knowledge of host factors co-opted and signaling pathways activated
during HCoV infection, with an emphasis on HCoV-infection-induced stress
response, autophagy, apoptosis, and innate immunity. The cross talk
among these pathways, as well as the modulatory strategies utilized by
HCoV, is also discussed.
Coronavirus humano: Interacción huésped-patógeno
Extracto
La infección por el coronavirus humano (HCoV) causa enfermedades respiratorias con resultados de leves a severos. En los últimos 15 años, hemos sido testigos de la aparición de dos HCoV zoonóticos y altamente patógenos: el coronavirus del síndrome respiratorio agudo severo (SARS-CoV) y el coronavirus del síndrome respiratorio de Oriente Medio (MERS-CoV). La replicación del HCoV está regulada por una diversidad de factores del huésped e induce alteraciones drásticas en la estructura y fisiología celular. La activación de vías de señalización críticas durante la infección por HCoV modula la inducción de la respuesta inmunológica antiviral y contribuye a la patogénesis del HCoV. Estudios recientes han comenzado a revelar algunos aspectos fundamentales de la intrincada interacción entre el HCoV y el huésped en detalles mecánicos. En esta revisión, resumimos el conocimiento actual de los factores del huésped cooptados y las vías de señalización activadas durante la infección por HCoV, con énfasis en la respuesta al estrés inducido por la infección por HCoV, la autofagia, la apoptosis y la inmunidad innata. También se examina el cruce de estas vías, así como las estrategias moduladoras utilizadas por el HCoV.
Conclusiones
Como parásitos intracelulares obligados y restringidos por sus limitadas capacidades genómicas, todos los virus han evolucionado para secuestrar los factores del huésped y facilitar su replicación. Mientras tanto, las células huéspedes también han desarrollado intrincadas redes de señalización para detectar, controlar y erradicar los virus intrusos, aunque estas vías antivirales suelen ser evadidas, inhibidas o subvertidas por diversos contramecanismos virales. La interacción entre virus y huéspedes representa, por lo tanto, una carrera armamentística evolutiva en curso que se ha perfeccionado a nivel molecular y celular. En este examen hemos resumido los progresos recientes en los estudios sobre la interacción entre el HCoV y el huésped, haciendo hincapié en los factores de huésped cooptado y las vías de señalización críticas. Evidentemente, cada paso del ciclo de replicación del HCoV involucra ciertos factores del huésped, y las dramáticas alteraciones en la estructura y fisiología celular activan la respuesta de estrés del huésped, la autofagia, la apoptosis y la inmunidad innata. Con los recientes avances en el análisis multiómico y la edición del genoma (como el CRISPR), es muy probable que en el futuro se descubran y caractericen cada vez más factores del huésped y vías implicadas en la infección por HCoV. Estos estudios, complementados con los diversos modelos animales de HCoV bien establecidos y los sistemas de genética inversa, es de esperar que desentrañen mecanismos anteriormente desconocidos que subyacen a la biología molecular del HCoV y cómo interactúan con el huésped.
Desde una perspectiva práctica, el estudio de la interacción entre el HCoV y el huésped también es fundamental ante la posible aparición y/o resurgimiento futuro del HCoV altamente patógeno. En los últimos 15 años, hemos sido testigos de brotes de dos HCoV zoonóticos y altamente patógenos. Los graves síntomas observados en los pacientes con SARS y MERS son, en efecto, en gran parte debidos a las inmunopatías, debido a la activación aberrante del sistema inmunológico. En cambio, otros HCoV leves causan infecciones autolimitadas del tracto respiratorio superior, que sólo en raras ocasiones se convierten en enfermedades que ponen en peligro la vida de los individuos inmunocomprometidos. ¿Cómo pueden estos virus relacionados manifestarse de forma tan diferente en términos de patogénesis? Hasta cierto punto, esto puede explicarse por los diferentes patrones de interacción de la HCoV con las células huésped. Un ejemplo es que los HCoV leves suelen inducir un alto nivel de producción de IFN-I, mientras que se sabe que el SARS-CoV y el MERS-CoV antagonizan la inducción y la señalización de interferón mediante numerosos mecanismos. Una mejor comprensión de la interacción entre el HCoV y el huésped permitirá determinar con precisión los factores virales y de huésped críticos que controlan la patogénesis del HCoV y desarrollar enfoques terapéuticos más eficaces contra la infección por el HCoV. Por ejemplo, es menos probable que los medicamentos dirigidos a los factores esenciales del huésped se seleccionen para las variantes del HCoV resistentes a los medicamentos. Además, aunque la respuesta inmunológica hiperactiva debe suprimirse en las enfermedades graves causadas por el HCoV, el aumento de la activación del sistema inmunológico sería beneficioso durante la administración de la vacuna. Por último, los hallazgos sobre la interacción entre el HCoV y el huésped también pueden extrapolarse a otros coronavirus animales y zoonóticos, lo que arrojará nueva luz sobre la prevención y el control de estos patógenos de importancia económica y veterinaria, así como sobre la aparición de nuevos patógenos coronavirales zoonóticos.
INTRODUCTION
Coronaviruses
are a group of enveloped viruses with nonsegmented, single-stranded,
and positive-sense RNA genomes. Apart from infecting a variety of
economically important vertebrates (such as pigs and chickens), six
coronaviruses have been known to infect human hosts and cause
respiratory diseases. Among them, severe acute respiratory syndrome
coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus
(MERS-CoV) are zoonotic and highly pathogenic coronaviruses that have
resulted in regional and global outbreaks.
-
Los coronavirus son un grupo de virus envueltos con genomas de ARN no segmentados, de una sola cadena y de sentido positivo. Además de infectar a diversos vertebrados económicamente importantes (como cerdos y pollos), se sabe que seis coronavirus infectan a huéspedes humanos y causan enfermedades respiratorias. Entre ellos, el coronavirus del síndrome respiratorio agudo severo (SARS-CoV) y el coronavirus del síndrome respiratorio del Oriente Medio (MERS-CoV) son coronavirus zoonóticos y altamente patógenos que han dado lugar a brotes regionales y mundiales
-
According to the International Committee on Taxonomy of Viruses, coronaviruses are classified under the order
Nidovirales, family
Coronaviridae, subfamily
Coronavirinae. Based on early serological and later genomic evidence,
Coronavirinae is divided into four genera:
Alphacoronavirus,
Betacoronavirus,
Gammacoronavirus, and
Deltacoronavirus (
126). Four distinct lineages (A, B, C, and D) have been assigned within the genus
Betacoronavirus. Among the six known human coronaviruses (HCoVs), HCoV-229E and HCoV-NL63 belong to
Alphacoronavirus, whereas HCoV-OC43 and HCoV-HKU1 belong to lineage A, SARS-CoV to lineage B, and MERS-CoV to lineage C
Betacoronavirus (
Figure 1).
In
November 2002, a viral respiratory disease first appeared in southern
China and quickly spread to other countries, leading to over 8,000
confirmed cases at the end of the epidemic in June 2003, with a
mortality rate of ∼9.6% (
98).
The etiologic agent was identified as SARS-CoV, a zoonotic
betacoronavirus originated in horseshoe bats that later adapted to
infect the intermediate host palm civet and ultimately humans (
64).
After an incubation period of 4–6 days, SARS patients develop flu-like
symptoms and pneumonia, which in severe cases lead to fatal respiratory
failure and acute respiratory distress syndrome (
96).
Although SARS-CoV infects multiple organs and causes systemic disease,
symptoms indeed worsen as the virus is cleared, suggesting that aberrant
immune response may underlie the pathogenesis of SARS-CoV (
98).
While no cases of SARS have been reported since 2004, a rich gene pool
of bat SARS-related coronaviruses was discovered in a cave in Yunnan,
China, highlighting the necessity to prepare for future reemergence (
50).
In June 2012, MERS-CoV emerged in Saudi Arabia as the causative agent of a SARS-like respiratory disease (
25).
Although human-to-human transmission is considered limited, MERS-CoV
has caused two major outbreaks in Saudi Arabia (2012) and South Korea
(2015), with the global confirmed cases exceeding 2,000 and a mortality
rate of ∼35% (
10).
Elderly people infected with MERS-CoV, particularly those with
comorbidities, usually develop more severe and sometimes fatal disease (
42). Similar to SARS-CoV, MERS-CoV originated in bats, but it later adapted to dromedary camels as intermediate hosts (
17). Currently, no vaccine or specific antiviral drug has been approved for either SARS-CoV or MERS-CoV.
Prior
to the emergence of SARS-CoV, only two HCoVs (HCoV-229E and HCoV-OC43)
were known, both causing mild upper respiratory symptoms when inoculated
to healthy adult volunteers (
45). Two more HCoVs, HCoV-NL63 and HCoV-HKU1, were identified in 2004 and 2005, respectively (
31,
127). Together, these four globally distributed HCoVs presumably contribute to 15–30% of cases of common cold in humans (
69).
Although diseases are generally self-limiting, these mild HCoVs can
sometimes cause severe lower respiratory infections in infants, elderly
people, or immunocompromised patients (
41,
97).
Similar to SARS-CoV and MERS-CoV, HCoV-NL63 and HCoV-229E originated in
bats, whereas HCoV-OC43 and HCoV-HKU1 likely originated in rodents (
22).
Importantly, a majority of alphacoronaviruses and betacoronaviruses
were identified only in bats, and many coronaviruses phylogenetically
related to SARS-CoV and MERS-CoV were discovered in diverse bat species (
22).
Therefore, emerging zoonotic HCoVs such as SARS-CoV and MERS-CoV likely
originated in bats through sequential mutation and recombination of bat
coronaviruses, underwent further mutations during the spillover to
intermediate hosts, and finally acquired the ability to infect human
hosts (
22).
In
this review, we first revisit the replication cycle of HCoV, with a
particular focus on the host factors co-opted during individual stages
of HCoV replication. Next, we summarize the current knowledge of
important signaling pathways activated during HCoV infection, including
stress response, autophagy, apoptosis, and innate immunity. The cross
talk among these pathways and the modulatory strategies utilized by HCoV
are also discussed.
HCoV REPLICATION AND THE INVOLVEMENT OF HOST FACTORS
Morphology and Genomic Structure of HCoV
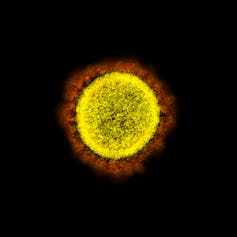
Coronaviruses
are spherical or pleomorphic, with a diameter of 80–120 nm. Under the
electron microscope, the virion surface is decorated with club-like
projections constituted by the trimeric spike (S) glycoprotein (
79).
Shorter projections made up of the dimeric hemagglutinin-esterase (HE)
protein are observed in some betacoronaviruses (such as HCoV-OC43 and
HCoV-HKU1) (
24).
Both S and HE are type I transmembrane proteins with a large ectodomain
and a short endodomain. The viral envelope is supported by the membrane
(M) glycoprotein, the most abundant structural protein that embeds in
the envelope via three transmembrane domains (
79).
Additionally, a small transmembrane protein known as the envelope (E)
protein is also present in a low amount in the envelope (
71).
Finally, the nucleocapsid (N) protein binds to the RNA genome in a
beads-on-a-string fashion, forming the helically symmetric nucleocapsid (
79).
The
coronavirus genome is a positive-sense, nonsegmented, single-stranded
RNA, with an astoundingly large size ranging from 27 to 32 kilobases.
The genomic RNA is 5′-capped and 3′-polyadenylated and contains multiple
open reading frames (ORFs). The invariant gene order is
5′-replicase-S-E-M-N-3′, with numerous small ORFs (encoding accessory
proteins) scattered among the structural genes (
Figure 2).
The coronavirus replicase is encoded by two large overlapping ORFs
(ORF1a and ORF1b) occupying about two-thirds of the genome and is
directly translated from the genomic RNA. The structural and accessory
genes, however, are translated from subgenomic RNAs (sgRNAs) generated
during genome transcription/replication as described below.
The
coronavirus replication cycle is divided into several steps: attachment
and entry, translation of viral replicase, genome transcription and
replication, translation of structural proteins, and virion assembly and
release (
Figure 3). In this section, we briefly review each step and summarize host factors involved in coronavirus replication (
Table 1).
Attachment and Entry
Coronavirus
replication is initiated by the binding of S protein to the cell
surface receptor(s). The S protein is composed of two functional
subunits, S1 (bulb) for receptor binding and S2 (stalk) for membrane
fusion. Specific interaction between S1 and the cognate receptor
triggers a drastic conformational change in the S2 subunit, leading to
the fusion between the virus envelope and the cellular membrane and
release of the nucleocapsid into the cytoplasm (
79).
Receptor binding is the major determinant of host range and tissue
tropism for a coronavirus. Some HCoVs have adopted cell surface enzymes
as receptors, such as aminopeptidase N (APN) for HCoV-229E, angiotensin
converting enzyme 2 (ACE2) for HCoV-NL63 and SARS-CoV, and dipeptidyl
peptidase 4 (DPP4) for MERS-CoV, while HCoV-OC43 and HCoV-HKU1 use 9-
O-acetylated sialic acid as a receptor (
69).
The
S1/S2 cleavage of coronavirus S protein is mediated by one or more host
proteases. For instance, activation of SARS-CoV S protein requires
sequential cleavage by the endosomal cysteine protease cathepsin L (
7,
105) and another trypsin-like serine protease (
4). On the other hand, the S protein of MERS-CoV contains two cleavage sites for a ubiquitously expressed protease called furin (
84).
Interestingly, whereas the S1/S2 site was cleaved during the synthesis
of MERS-CoV S protein, the other site (S2′) was cleaved during viral
entry (
84).
A similar cleavage event was also observed in infectious bronchitis
virus (IBV), a prototypic gammacoronavirus that infects chickens, in an
earlier study (
132).
Additionally, type II transmembrane serine proteases TMPRSS2 and
TMPRSS11D have also been implicated in the activation of S protein of
SARS-CoV (
6) and HCoV-229E (
5).
Apart from S activation, host factors might also be involved in
subsequent stages of virus entry. For example, valosin-containing
protein (VCP) contributed to the release of coronavirus from early
endosomes, as knockdown of VCP led to decreased replication of both
HCoV-229E and IBV (
125).
Host
factors could also restrict the attachment and entry of HCoV. For
example, interferon-inducible transmembrane proteins (IFITMs) exhibited
broad-spectrum antiviral functions against various RNA viruses (
2). The entry of SARS-CoV, MERS-CoV, HCoV-229E, and HCoV-NL63 was restricted by IFITMs (
51). In sharp contrast, however, HCoV-OC43 used IFITM2 or IFITM3 as an entry factor to facilitate its infection (
144).
A recent study identified several amino acid residues in IFITMs that
control the restriction versus enhancing activities on HCoV entry (
145).
Translation of Replicase and Assembly of the Replication Transcription Complex
After
entry and uncoating, the genomic RNA serves as a transcript to allow
cap-dependent translation of ORF1a to produce polyprotein pp1a.
Additionally, a slippery sequence and an RNA pseudoknot near the end of
ORF1a enable 25–30% of the ribosomes to undergo −1 frameshifting,
thereby continuing translation on ORF1b to produce a longer polyprotein
pp1ab (
79).
The autoproteolytic cleavage of pp1a and pp1ab generates 15–16
nonstructural proteins (nsps) with various functions. Importantly, the
RNA-dependent RNA polymerase (RdRP) activity is encoded in nsp12 (
130), whereas papain-like protease (PLPro) and main protease (Mpro) activities are encoded in nsp3 and nsp5, respectively (
149). nsp3, 4, and 6 also induce rearrangement of the cellular membrane to form double-membrane vesicles (DMVs) or spherules (
1,
77), where the coronavirus replication transcription complex (RTC) is assembled and anchored.
Apart
from the RNA secondary structures, programmed ribosomal frameshifting
(PRF) might also be regulated by viral and/or host factors. For example,
PRF in the related arterivirus porcine reproductive and respiratory
syndrome virus (PRRSV) was transactivated by the viral protein nsp1β,
which interacts with the PRF signal via a putative RNA-binding motif (
65). A host RNA-binding protein called annexin A2 (ANXA2) was also shown to bind the pseudoknot structure in the IBV genome (
62).
In
terms of DMV formation and RTC assembly, host factors in the early
secretory pathway seemed to be involved. Golgi-specific brefeldin
A–resistance guanine nucleotide exchange factor 1 (GBF1) and its
effector ADP ribosylation factor 1 (ARF1) are both required for normal
DMV formation and efficient RNA replication of mouse hepatitis virus
(MHV), a prototypic betacoronavirus that infects mice (
119).
Genome Replication and Transcription
Using
the genomic RNA as a template, the coronavirus replicase synthesizes
full-length negative-sense antigenome, which in turn serves as a
template for the synthesis of new genomic RNA (
79).
The polymerase can also switch template during discontinuous
transcription of the genome at specific sites called
transcription-regulated sequences, thereby producing a 5′-nested set of
negative-sense sgRNAs, which are used as templates for the synthesis of a
3′-nested set of positive-sense sgRNAs (
79).
Although
genome replication/transcription is mainly mediated by the viral
replicase and confines in the RTC, the involvement of various host
factors has been implicated. For instance, coronavirus N protein is
known to serve as an RNA chaperone and facilitate template switching (
150,
151).
Importantly, the N protein of SARS-CoV and MHV-JHM was also
phosphorylated by glycogen synthase kinase 3 (GSK3), and inhibition of
GSK3 was shown to inhibit viral replication in Vero E6 cells infected
with SARS-CoV (
129).
Additionally, GSK3-mediated phosphorylation of the MHV-JHM N protein
recruited an RNA-binding protein DEAD-box helicase 1 (DDX1), which
facilitates template read-through, favoring the synthesis of genomic RNA
and longer sgRNAs (
128).
Another RNA-binding protein called heterogeneous nuclear
ribonucleoprotein A1 (hnRNPA1) can also bind tightly to SARS-CoV N
protein and potentially regulate viral RNA synthesis (
74).
Host
RNA-binding proteins could also bind directly to untranslated regions
(UTRs) of the coronavirus genome to modulate replication/transcription,
such as zinc finger CCHC-type and RNA-binding motif 1 (ZCRB1) binding to
the 5′-UTR of IBV (
111), mitochondrial aconitase binding to the 3′-UTR of MHV (
90), and poly(A)-binding protein (PABP) to the poly(A) tail of bovine coronavirus (
108).
Translation of Structural Proteins
Most
of the coronavirus sgRNAs are functionally monocistronic, and thus only
the 5′-most ORF is translated in a cap-dependent manner (
79).
However, some sgRNAs can also employ other mechanisms, such as ribosome
leaky scanning and ribosome internal entry, to translate additional
ORFs (
71).
Transmembrane structural proteins (S, HE, M, and E) and some
membrane-associated accessory proteins are translated in the ER, whereas
the N protein is translated by cytosolic free ribosomes (
79).
Recent studies using ribosome profiling have identified ribosome pause
sites and revealed several short ORFs upstream of, or embedded within,
known viral protein-encoding regions (
52).
Most coronavirus structural proteins are subjected to posttranslational modifications that modulate their functions (
40). For example, both S and M proteins were modified by glycosylation (
147). Although N-linked glycosylation of SARS-CoV S protein does not contribute to receptor binding (
109), it might be involved in lectin-mediated virion attachment (
46) and might constitute some neutralizing epitopes (
107). Also,
O-linked glycosylation of M protein affects the ability of MHV to induce type I interferon and its replication in mice (
26).
Proper folding and maturation of viral transmembrane proteins (in
particular S) also rely heavily on ER protein chaperones such as
calnexin (
33).
Virion Assembly and Release
Particle assembly occurs in the ER-Golgi intermediate compartment (ERGIC) and is orchestrated by the M protein (
57,
79).
Homotypic interaction of M protein provides the scaffold for virion
morphogenesis, whereas M-S and M-N interactions facilitate the
recruitment of structural components to the assembly site (
48). The E protein also contributes to particle assembly by interacting with M and inducing membrane curvature (
68).
Finally, coronavirus particles budded into the ERGIC are transported in
smooth-wall vesicles and trafficked via the secretory pathway for
release by exocytosis.
Various host factors have been implicated
in the assembly and release of coronavirus. In particular, interactions
between the cytoskeleton and structural proteins seem to be essential.
Interactions between tubulins and the cytosolic domain of S protein of
HCoV-229E, HCoV-NL63, and TGEV are required for successful assembly and
release of infectious viral particles (
103).
Similarly, interactions between IBV M protein and β-actin, between TGEV
N protein and vimentin (an intermediate filament protein), and between
TGEV S protein and filamin A (an actin-binding protein) have been shown
to facilitate coronavirus particle assembly and/or release (
121,
143).
ACTIVATION OF AUTOPHAGY DURING HCoV INFECTION
Macroautophagy
(hereafter referred to as autophagy) is a conserved cellular process
involving self (auto) eating (phagy). Specifically, cells under stress
conditions (such as starvation, growth factor deprivation, or infection
by pathogens) initiate autophagy in nucleation sites at the ER, where
part of the cytoplasm and/or organelles are sequestered in
autophagosomes and degraded by fusing with lysosomes (
135). Autophagy is tightly regulated by highly conserved autophagy-related genes (ATGs) (
Figure 4).
Autophagy
activation is yet to be characterized for human alphacoronavirus
infection. In the related porcine alphacoronavirus PEDV, autophagy was
activated in Vero cells infected with PEDV strain CH/YNKM-8/2013, and
autophagy inhibition suppressed viral replication and reduced the
production of proinflammatory cytokines (
44).
Similarly, activation of autophagy and mitophagy in porcine epithelial
cells (IPEC-J2) infected with TGEV (strain SHXB) benefited viral
replication and protected infected cells from oxidative stress and
apoptosis (
148).
In contrast, in two separate studies using swine testicular cells
infected with TGEV (strain H165) or IPEC-J2 cells infected with PEDV
(strain SM98), activation of autophagy indeed suppressed viral
replication (
43,
58).
Such discrepancies might arise from differences in cell lines and virus
strains, calling for more comprehensive in vivo studies.
As for
betacoronavirus, initial studies observed colocalization of autophagy
protein LC3 and Atg12 with MHV replicase protein nsp8, hinting that DMV
formation might utilize components of cellular autophagy (
99). However, MHV replication was not affected in ATG5
−/− mouse embryonic fibroblasts (MEFs) (
146). Also, replication of SARS-CoV was comparable in wild-type or ATG5
−/− MEFs overexpressing ACE2, suggesting that intact autophagy is not required for betacoronavirus replication (
104).
Later, it was shown that MHV co-opted the host machinery for
COPII-independent vesicular ER export to derive membranes for DMV
formation. This process required the activity of nonlipidated LC3 but
was independent of host autophagy (
101).
Such autophagy-independent activity of LC3 was also implicated in the
replication of equine arteritis virus (EAV) of the family
Arteriviridae (
89). Therefore, it is quite likely that other viruses in the
Nidovirales order share this LC3-hijacking strategy for replication.
Coronavirus nsp6 is a multipass transmembrane protein implicated in the formation of DMVs during SARS-CoV infection (
1).
Overexpression of nsp6 of IBV, MHV, or SARS-CoV activated the formation
of autophagosomes from the ER via an omegasome intermediate (
18).
However, autophagosomes induced by IBV infection or overexpression of
coronavirus nsp6 had smaller diameters compared with those induced by
starvation, indicating that nsp6 might also restrict the expansion of
autophagosomes (
19).
INDUCTION OF APOPTOSIS DURING HCoV INFECTION
Apoptosis
is one form of programmed cell death characterized by the highly
controlled dismantling of cellular structures, which are released in
membrane-bound vesicles (known as apoptotic bodies) that are engulfed by
neighboring cells or phagocytes (
114).
Due to its self-limited nature, apoptosis is not immunogenic, thereby
distinguishing it from necrotic cell death, where uncontrolled leakage
of cellular contents activates an inflammatory response.
Apoptosis can be activated by two pathways (
Figure 5). The intrinsic pathway is orchestrated by the B cell lymphoma 2 (Bcl2) family proteins (
114).
Among them, BAX and BAK are proapoptotic, channel-forming proteins that
increase the mitochondrial outer membrane permeability (MOMP), whereas
Bcl2-like proteins (such as Bcl2, Bcl-xL, and Mcl-1) are antiapoptotic
factors that inhibit this process. Under stressful conditions (DNA
damage, growth factor deprivation, etc.) BH3-only proteins are activated
to overcome the inhibitory effect of Bcl2-like proteins. The resulting
increase in MOMP leads to release of cytochrome
c and formation
of an apoptosome, thereby activating effector caspase 3/7. In the
extrinsic pathway, binding of the death ligands [such as FasL and tumor
necrosis factor-α (TNF-α)] to the cell surface death receptors (such as
Fas and TNF receptor 1) leads to the formation of death-inducing
signaling complex and activation of caspase 8, which either directly
activates effector caspases or engages in cross talk with the intrinsic
pathway by activating the BH3-only protein Bid (
114).
Apoptosis
induced by HCoV infection has been extensively investigated. In autopsy
studies, hallmarks of apoptosis were observed in SARS-CoV-infected
lung, spleen, and thyroid tissues (
61).
Also, apoptosis induced by infection of SARS-CoV, MERS-CoV, or other
HCoVs was described in various in vitro systems and animal models (
113,
136).
Apart from respiratory epithelial cells, HCoVs also infect and induce
apoptosis in a variety of other cell types. For example, HCoV-OC43
induced apoptosis in neuronal cells (
30), while MERS-CoV induced apoptosis in primary T lymphocytes (
15). HCoV-229E infection also causes massive cell death in dendritic cells, albeit independent of apoptosis induction (
82).
Collectively, induction of cell death in these immune cells explains
the lymphopenia observed in some HCoV diseases (such as SARS) and may
contribute to the suppression of host immune response.
Apoptosis
can be induced by multiple mechanisms in HCoV-infected cells. SARS-CoV
was shown to induce caspase-dependent apoptosis, which is dependent on
but not essential for viral replication, as treatment of pan-caspase
inhibitor z-VAD-FMK or overexpression of Bcl2 did not significantly
affect SARS-CoV replication (
36).
In contrast, although MERS-CoV infection of human primary T lymphocytes
was abortive, apoptosis was induced via activation of both intrinsic
and extrinsic pathways (
15).
Apoptosis in neuronal cells infected with HCoV-OC43 involved
mitochondrial translocation of BAX but was independent of caspase
activation (
30).
Apoptosis
was also induced in cells overexpressing SARS-CoV proteins, including
S, E, M, N, and accessory protein 3a, 3b, 6, 7a, 8a, and 9b (
70). Among them, SARS-CoV E and 7a protein activated the intrinsic pathway by sequestering antiapoptotic Bcl-X
L to the ER (
112).
Other proapoptotic mechanisms by SARS-CoV included interfering with
prosurvival signaling by M protein and the ion channel activity of E and
3a (
70).
HCoV infection also modulated apoptosis by activating ER stress
response and mitogen-activated protein kinase (MAPK) pathway, as
discussed in detail in the following sections.
ACTIVATION OF ENDOPLASMIC RETICULUM STRESS DURING HCoV INFECTION
ER
is a membranous organelle and the main site for synthesis, folding, and
modification of secreted and transmembrane proteins. Affected by the
extracellular environment and physiological status, the amount of
protein synthesized in the ER can fluctuate substantially. When the ER
folding capacity is saturated, unfolded proteins accumulate in the ER
and lead to ER stress. During HCoV infection, viral structural proteins
are produced in massive amounts. In particular, the S glycoprotein
relies heavily on the ER protein chaperones and modifying enzymes for
its folding and maturation (
33). Indeed, overexpression of SARS-CoV S alone was sufficient to induce a potent ER stress response (
11).
In addition, membrane reorganization for DMV formation and membrane
depletion for virion assembly may also contribute to ER stress during
HCoV infection (
38).
To
restore ER homeostasis, signaling pathways known as unfolded protein
response (UPR) will be activated. UPR consists of three interrelated
pathways, named after the transmembrane sensors: protein kinase
RNA-activated (PKR)-like ER protein kinase (PERK), inositol-requiring
enzyme 1 (IRE1), and activating transcription factor 6 (ATF6) (
Figure 6). In the following section, activation of the three UPR branches by HCoV infection is discussed.
PERK Pathway and Integrated Stress Response
The
PERK pathway is the first to be activated among the three UPR branches.
In the stressed ER, protein chaperone GRP78 binds to unfolded proteins
and dissociates from the luminal domain of PERK, leading to
oligomerization and activation of PERK by autophosphorylation. Activated
PERK phosphorylates the α subunit of eukaryotic initiation factor 2
(eIF2α), which inhibits the conversion of inactive GDP-bound eIF2α back
to the active GTP-bound form, thereby suppressing translation
initiation. The resulting global attenuation of protein synthesis
reduces the ER protein influx and allows the ER to reprogram for
preferential expression of UPR genes. Besides PERK, eIF2α can also be
phosphorylated by three other kinases: heme-regulated inhibitor kinase
(HRI), general control nonderepressible 2 (GCN2), and PKR. PKR is an
interferon-stimulated gene (ISG) activated by binding of double-stranded
RNA (dsRNA), a common intermediate during the replication of DNA and
RNA viruses. Together, these four eIF2α kinases and their convergent
downstream signaling pathways are known as the integrated stress
response (ISR) (
102).
Although global protein synthesis is attenuated under ISR, a subset of genes is preferentially translated (
102).
One of them is activating transcription factor 4 (ATF4), a basic
leucine zipper (bZIP) transcription factor that switches on UPR effector
genes. ATF4 also induces another bZIP protein C/EBP-homologous protein
(CHOP), which is responsible for triggering apoptosis in cells under
prolonged ER stress. ATF4 and CHOP further induce growth arrest and DNA
damage–inducible protein 34 (GADD34), a regulatory subunit of protein
phosphatase 1 (PP1) that dephosphorylates eIF2α. This negative feedback
mechanism enables protein synthesis to resume after resolution of ER
stress.
In one early study, phosphorylation of PKR, PERK, and eIF2α was observed in 293/ACE2 cells infected with SARS-CoV (
61).
Surprisingly, knockdown of PKR had no effect on SARS-CoV replication or
virus-induced eIF2α phosphorylation, although SARS-CoV-induced
apoptosis was significantly reduced. These data suggested that
SARS-CoV-induced PKR activation might trigger apoptosis independent of
eIF2α phosphorylation (
61).
As detailed in the section titled Innate Immunity and Proinflammatory
Response, recent studies showed that the endoribonuclease activity of
coronavirus nsp15 and dsRNA-binding activity of MERS-CoV protein 4a
could also suppress PKR activation (
28,
56,
100).
Activation of ISR by other HCoVs is not fully understood. In neurons
infected with HCoV-OC43, only transient eIF2α phosphorylation was
observed at early infection, with no induction of ATF4 and CHOP (
30).
As
for animal coronaviruses, MHV-A59 infection induced significant eIF2α
phosphorylation and ATF4 upregulation, but the CHOP/GADD34/PP1
negative-feedback loop was not activated, leading to a sustained
translation attenuation (
3).
TGEV infection also induced eIF2α phosphorylation, and TGEV accessory
protein 7 interacted with PP1 and alleviated translation attenuation by
promoting eIF2α dephosphorylation (
21).
Finally, IBV infection triggered transient PKR, PERK, and eIF2α
phosphorylation at early infection, which was rapidly inactivated by
GADD34/PP1-mediated negative feedback (
66,
123).
Nonetheless, accumulation of CHOP promoted IBV-induced apoptosis,
presumably by inducing proapoptotic protein tribbles homolog 3 (TRIB3)
and suppressing the prosurvival extracellular regulated kinase 1/2
(ERK1/2) (
66).
IRE1 Pathway
Besides
being activated like PERK via dissociation of GRP78, IRE1 is also
activated by direct binding of the unfolded protein to its N-terminal
luminal domain (
20).
Upon activation by oligomerization and autophosphorylation, the
cytosolic RNase domain of IRE1 mediates an unconventional splicing of
the mRNA of X-box-binding protein 1 (XBP1) (
138).
The spliced and frameshifted transcript encodes XBP1S, a bZIP
transcription factor inducing the expression of numerous UPR effector
genes that enhance ER folding capacity (
134).
On the other hand, the unspliced transcript encodes XBP1U, a highly
unstable protein that negatively regulates XBP1S activity (
116).
Under prolonged ER stress, the RNase domain of IRE1 can also degrade
ER-associated mRNAs in a process called IRE1-dependent mRNA decay (RIDD)
(
49).
Although RIDD facilitates ER homeostasis by reducing ER-associated
mRNA, degradation of mRNAs encoding prosurvival proteins contributes to
ER-stress-induced cell death (
81).
Finally, the kinase activity of IRE1 also activates a signaling cascade
that ultimately activates c-Jun N-terminal kinase (JNK) (
118). Activation of the IRE1-JNK pathway is required for induction of autophagy and apoptosis in cells under ER stress (
93).
In one early study, overexpression of MHV S protein was found to induce XBP1 mRNA splicing (
120).
Also, infection with MHV-A59 induced XBP1 mRNA splicing, although XBP1S
protein was not produced, presumably due to translation suppression by
the PERK/PKR-eIF2α pathway (
3). In sharp contrast, neither SARS-CoV infection nor overexpression of SARS-CoV S protein could induce XBP1 mRNA splicing (
27,
120).
However, when the SARS-CoV E gene was deleted by reverse genetics, the
recombinant virus efficiently induced XBP1 mRNA splicing and upregulated
stress-induced genes, leading to a more pronounced apoptosis compared
with wild-type control (
27).
Thus, SARS-CoV E protein might serve as a virulent factor that
suppressed activation of the IRE1 pathway and SARS-CoV-induced
apoptosis. Infection with another
Betacoronavirus HCoV-OC43 induced XBP1 mRNA splicing and upregulation of downstream UPR effector genes (
30).
Notably, two point mutations in the S protein were reproducibly
observed during persistent infection of HCoV-OC43 in human neural cell
lines. Compared with wild-type control, recombinant HCoV-OC43 harboring
these two mutations induced a higher degree of XBP1 mRNA splicing and
apoptosis (
30). Taken together, activation of the IRE1 pathway seems to promote apoptosis during HCoV infection.
Efficient XBP1 mRNA splicing and upregulation of UPR effector genes were also observed in cells infected with IBV (
37).
In contrast with its role during HCoV infection, IRE1 indeed suppressed
apoptosis in IBV-infected cells, presumably by converting proapoptotic
XBP1U to antiapoptotic XBP1S, and by modulating phosphorylation of key
kinases such as JNK and AKT (
37).
ATF6 Pathway
Similar
to PERK and IRE1, ATF6 is activated by ER stress-induced dissociation
from GRP78. Alternatively, underglycosylation or reduction of disulfide
bonds in its ER luminal domain can also activate ATF6 (
69).
Upon activation, ATF6 is translocated to the Golgi apparatus, where
protease cleavage releases its N-terminal cytosolic domain (ATF6-p50).
ATF6-p50 is a bZIP transcription factor that translocates to the nucleus
and induces the expression of UPR effector genes harboring ER stress
response element (ERSE) or ERSE-II in the promoters (
139).
Apart from ER protein chaperones, ATF6 also induces the expression of
CHOP and XBP1, thereby connecting the three UPR branches into an
integrated signaling network (
102).
Activation
of the ATF6 pathway by HCoV infection is less studied, and most studies
have relied on indirect methods, such as luciferase reporter, due to
the lack of a specific antibody. No ATF6 cleavage was detected in cells
infected with SARS-CoV (
27), and overexpression of SARS-CoV S protein failed to activate ATF6 luciferase reporter (
11).
However, ATF6 cleavage and nuclear translocation were observed in cells
transfected with SARS-CoV accessory protein 8ab, and physical
interaction between 8ab and the luminal domain of ATF6 was also
determined (
110).
The SARS-CoV 8ab protein was only detected in early isolates during the
pandemic, while two separated proteins 8a and 8b were encoded in later
isolates resulting from a 29-nucleotide genome deletion (
94).
ACTIVATION OF MAPK PATHWAYS DURING HCoV INFECTION
MAPKs
are evolutionarily conserved serine/threonine protein kinases, which
are activated in response to a variety of environmental stimuli, such as
heat shock, DNA damage, and the treatment with mitogens or
proinflammatory cytokines (
55).
MAPKs are currently classified into four groups, namely ERK1/2, ERK5,
p38, and JNK. To become activated, MAPKs require dual phosphorylation of
threonine and tyrosine by upstream MAPK kinases (MKKs) within a
conserved TxY motif. MKKs are in turn activated by MKK kinases (MKKKs,
also known as MAP3Ks). MAP3Ks are usually activated in multiple steps
and regulated by complex mechanisms, such as allosteric inhibition
and/or activation by yet other kinases (MAP4Ks) (
55).
Because MKKs have high substrate specificity toward the cognate MAPKs,
classical MAPK signaling pathways are typically multi-tiered and linear.
However, some levels of signaling cross talk do occur, and some
atypical MAPKs can be directly activated by MAP3K. By phosphorylating
their protein substrates (in many cases transcription factors),
activated MAPKs regulate numerous critical cellular processes such as
proliferation, differentiation, apoptosis, and immune response (
55). The activation of p38, ERK, and JNK pathways during HCoV infection is discussed below (
Figure 7).
p38 Pathway
Activated
p38 translocates to the nucleus and directly or indirectly
phosphorylates a broad range of substrate proteins, including important
transcription factors such as cAMP response element-binding protein
(CREB), ATF1, signal transducer and activator of transcription 1
(STAT1), and STAT3 (
140).
By mediating the phosphorylation of eIF4E, activated p38 can suppress
the initiation of protein translation. The p38 pathway may also regulate
apoptosis by phosphorylating of p53 or other proapoptotic proteins such
as CHOP (
8,
124).
In
early studies, phosphorylation of p38, its upstream kinase MKK3/6, and
its downstream substrates was detected in Vero E6 cells infected with
SARS-CoV (
85,
86).
Specifically, p38-dependent phosphorylation of eIF4E might contribute
to the suppression of cellular protein synthesis during SARS-CoV
infection. However, SARS-CoV genome replication and viral protein
synthesis were not affected by the treatment with p38 inhibitor,
suggesting that p38 phosphorylation was not essential during SARS-CoV
infection in cell culture (
86).
Notably, overexpression of SARS-CoV accessory protein 7a alone could
induce p38 phosphorylation and inhibit cellular protein synthesis (
60).
Moreover, activation of the p38 pathway was also implicated in
apoptosis induced by overexpression of SARS-CoV protein 3a or 7a (
60,
95).
Phosphorylation of p38 was also observed in human fetal lung cells L132
infected with HCoV-229E, and p38 inhibition was found to inhibit
HCoV-229E replication (
59). Activation of the p38 pathway was also observed in cells infected with feline coronavirus (FCoV), TGEV, MHV, or IBV (
34).
ERK Pathway
Similar
to p38, activated ERK also exerts its function by phosphorylating
numerous transcription factors, such as ATF2, c-Fos, and Bcl6 (
137).
Unlike p38, activated ERK mediates the phosphorylation eIF4E binding
protein 1 (eIF4EBP1), causing its dissociation from eIF4E and thereby
promoting protein synthesis. ERK also directly phosphorylates 90-kDa
ribosomal protein S6 kinases (p90RSKs), which are important kinases
regulating protein translation and cell proliferation (
32). ERK also regulates Bcl2 family proteins such as BAD, thereby suppressing apoptosis and promoting cell survival (
137).
In an early study, phosphorylation of ERK and upstream kinases MKK1/2 was observed in Vero E6 cells infected with SARS-CoV (
85).
In fact, incubation of A549 cells with SARS-CoV S protein or SARS-CoV
virus-like particles was sufficient to induce ERK phosphorylation (
14). However, activation of p90RSK, one of the key substrates of ERK, was complicated in SARS-CoV-infected cells (
88).
Upon mitogen stimulation, p90RSK is first phosphorylated by ERK at
Thr573 at the C terminus, which leads to autophosphorylation at Ser380.
This then allows for the binding of another kinase that phosphorylates
p90RSK at Ser221 in the N terminus, leading to its full activation (
23). Interestingly, a basal level of Thr573 phosphorylation in p90RSK was abolished in SARS-CoV-infected Vero E6 cells (
88).
On the other hand, phosphorylation of p90RSK at Ser380 was
significantly induced by SARS-CoV infection, which was dependent on the
activation of the p38 pathway (
88).
Therefore, activation of p90RSK might adopt a completely different
mechanism in SARS-CoV-infected cells, involving potential cross talk
between the ERK and p38 pathways. The same study also observed that
treatment with MKK1/2 inhibitor had no effect on SARS-CoV-induced
apoptosis, suggesting that activation of the ERK pathway was not
sufficient to antagonize apoptosis during SARS-CoV infection (
88). This is different from infection with IBV, where ERK apparently served as an antiapoptotic factor (
66). Finally, activation of the ERK pathway was also observed in cells infected with MERS-CoV and HCoV-229E (
69).
JNK Pathway
Similar
to p38 and ERK, active JNK translocates to the nucleus to phosphorylate
a number of transcription factors such as c-Jun and ATF2 (
106).
Phosphorylated c-Jun then dimerizes with other proteins to form the
activator protein 1 (AP-1) complex, which binds to promoters with 12-
O-tetradecanoylphobol-13-acetate response element (TRE) and activates gene expression (
47). Besides inducing the transcription of proapoptotic genes such as
Bak and
FasL
in the nucleus, JNK also translocates to the mitochondria and directly
phosphorylates Bcl2 family proteins, thereby promoting stress-induced
apoptosis (
133).
Phosphorylation of JNK and its upstream kinases MKK4 and MKK7 was observed in Vero E6 cells infected with SARS-CoV (
87).
Additionally, JNK phosphorylation was detected in 293T cells
overexpressing SARS-CoV S protein, mediated by protein kinase C epsilon
in a calcium-independent pathway (
72).
Interestingly, treatment with JNK inhibitor abolished persistent
infection of SARS-CoV in Vero E6 cells, suggesting a prosurvival
function of the JNK pathway (
87).
This is quite unexpected because apoptosis induced by overexpression of
SARS-CoV N or accessory protein 6 or 7a was JNK dependent (
69), and activation of JNK also promoted IBV-induced apoptosis (
37,
39).
Presumably JNK might be proapoptotic during initial SARS-CoV infection
but later switched to a prosurvival role in persistently infected cells.
INNATE IMMUNITY AND PROINFLAMMATORY RESPONSE
The
innate immune system is a conserved defense strategy critical for the
initial detection and restriction of pathogens and later activation of
the adaptive immune response. Effective activation of innate immunity
relies on the recognition of pathogen-associated molecular patterns
(PAMPs) by pattern recognition receptors (PRRs), such as Toll-like
receptors (TLRs) and RIG-I-like receptors (RLRs) (
69).
Upon activation by PAMPs, PRRs recruit adaptor proteins, which initiate
complicated signaling pathways involving multiple kinases. This
ultimately leads to the activation of crucial transcription factors
including interferon regulatory factor 3 (IRF3), nuclear factor
kappa-light-chain-enhancer of activated B cells (NF-κB), and AP-1.
Synergistically, these factors promote the production of type I
interferons (IFN-I), which are released and act on neighboring cells by
binding to IFN-α/β receptor (IFNAR) (
69).
The antiviral activity of IFN-I is mediated by the induction of
numerous interferon-stimulated genes (ISGs), which antagonize viral
replication by various mechanisms (
Figure 8).
Meanwhile, cytokines and chemokines are also induced to activate an
inflammatory response, which is also sometimes responsible for extensive
tissue damage and other immunopathies associated with HCoV infection (
98).
While mild HCoVs such as HCoV-229E typically induced a high level of IFN-I production (
82),
SARS-CoV and MERS-CoV were shown to utilize numerous mechanisms to
suppress the activation of host innate immune response. Several
structural proteins (M and N), nonstructural proteins (nsp1 and nsp3),
and accessory proteins of SARS-CoV and/or MERS-CoV were identified as
interferon antagonists (
40,
69,
70).
In the following section, the involvement of UPR/ISR and MAPK in
HCoV-induced innate immunity is discussed, followed by two important
strategies utilized by HCoV to modulate the innate immune response.
Involvement of ER Stress and ISR
UPR
pathways may modulate innate immune and cytokine signaling by multiple
mechanisms, including activation of NF-κB and cross talk with MAPK
pathways (
38).
Also, PKR/eIF2α/ATF4-dependent upregulation of GADD34 was essential for
the production of interferon beta (IFN-β) and interleukin 6 (IL-6)
induced by polyI:C or chikungunya virus infection (
16).
Moreover, UPR transcription factors such as XBP1 may directly bind to
the promoter/enhancer of IFN-β and IL-6 to activate transcription (
78).
Recently, it was found that while the PERK branch of UPR suppressed
TGEV replication by activating NF-κB-dependent IFN-I production (
131), the IRE1 branch indeed facilitated IFN-I evasion by downregulating the expression level of miRNA miR-30a-5p (
75). Whether similar mechanisms apply during HCoV infection will require further investigation.
Another
important antiviral protein in innate immunity is PKR, which requires
dsRNA binding for full activation. In a recent study, endoribonuclease
(EndoU) activity encoded by coronavirus nsp15 was found to efficiently
suppress the activation of host dsRNA sensors including PKR (
56).
Replication of EndoU-deficient MHV was greatly attenuated and
restricted in vivo even during the early phase of infection. It also
triggered an elevated interferon response and induced PKR-dependent
apoptosis (
28,
56).
Moreover, EndoU-deficient coronavirus also effectively activated MDA5
and OAS/RNase L, caused attenuated disease in vivo, and stimulated a
protective immune response (
28). Interestingly, protein 4a (p4a) of MERS-CoV was also identified as a dsRNA-binding protein (
100).
By sequestering dsRNA, MERS-CoV p4a suppressed PKR-dependent
translational inhibition, formation of stress granules, and the
activation of interferon signaling (
100).
Involvement of MAPK
The
MAPK pathways contribute to innate immunity mainly by activating AP-1
and other transcription factors regulating the expression of
proinflammatory cytokines. For instance, activation of p38 was essential
for cytokine production and immunopathology in mice infected with
SARS-CoV (
53).
Also, upregulation and release of CCL2 and IL-8 induced by the binding
of SARS-CoV S protein was dependent on the activation of ERK (
12,
14).
Similarly, the JNK pathway was required for the induction of
cyclooxygenase 2 (COX-2) and IL-8 in cells overexpressing SARS-CoV S
protein (
12,
72).
Similar involvement of MAPK pathway in the induction of proinflammatory
cytokines (such as IL-6, IL-8, and TNF-α) was determined for numerous
animal coronaviruses as well (
34).
In addition, MAPK may also regulate cytokine signaling. For example,
SARS-CoV infection caused dephosphorylation of STAT3 at Tyr705 in VeroE6
cells, leading to its nuclear exclusion (
85).
Inhibition of p38 partially inhibited this process, suggesting a
suppressive role of p38 in STAT3 signaling during SARS-CoV infection (
85).
Deubiquitinating and deISGylating Activity of HCoV PLPro
Coronaviruses
typically encode one or two PLPros in nsp3. Besides the
polyprotein-cleaving protease activity, deubiquitinating activity was
also identified for PLPro of SARS-CoV, MERS-CoV, and IBV, as well as
PLP2 of HCoV-NL63 and MHV-A59 (
40).
Additionally, PLPro of SARS-CoV and MERS-CoV also recognized proteins
modified by ISG15 and catalyzed its removal (deISGylation) (
83).
Expectedly, deubiquitination and deISGylation of critical factors in
the innate immune signaling were utilized by HCoV to antagonize host
antiviral response. For instance, overexpressing PLPro of SARS-CoV or
MERS-CoV significantly reduced the expression of IFN-β and
proinflammatory cytokines in MDA5-stimulated 293T cells (
83).
Also, SARS-CoV PLPro catalyzed deubiquitination of
TNF-receptor-associated factor 3 (TRAF3) and TRAF6, thereby suppressing
IFN-I and proinflammatory cytokines induced by TLR7 agonist (
63).
The deubiquitinating activity of SARS-CoV PLPro also suppressed a
constitutively active phosphomimetic IRF3, suggesting its involvement in
the postactivation signaling of IRF3 (
80).
Nonetheless, HCoV PLPro could also antagonize innate immunity by
mechanisms independent of its deubiquitinating/deISGylating activity (
29).
Ion Channel Activity and PDZ-Binding Motif of Viroporins Encoded by HCoV
Viroporins
are small hydrophobic viral proteins that oligomerize to form ion
channels on cellular membrane and/or virus envelope. They are encoded by
a wide range of viruses from different families (
35). For coronaviruses, ion channel activity has been described for the E protein of MHV (
76), SARS-CoV (
67), and IBV (
117); 3a (
73) and 8a (
13) of SARS-CoV; ORF3 of PEDV (
122); ORF4a of HCoV-229E (
141); and ns12.9 of HCoV-OC43 (
142).
Ion
channel activity is essential for viral replication for some
coronaviruses. For instance, recombinant IBV harboring ion
channel–defective mutation T16A or A26F in the E gene produced similar
intracellular viral titers but released a significantly lower level of
infectious virions to the supernatant, suggesting that ion channel
activity might specifically contribute to IBV particle release (
117).
Similarly, compared with wild-type HCoV-OC43, recombinant virus lacking
ns12.9 suffered a tenfold reduction of virus titer in vivo and in vitro
(
142).
Unlike IBV, however, intracellular titers of HCoV-OC43-Δns12.9 were
markedly reduced, and electron microscopy suggested defective virion
morphogenesis (
142). Experiments using small interfering RNA (siRNA) also showed that silencing SARS-CoV 3a (
73), HCoV-229E ORF4a (
141), or PEDV ORF3 (
122)
resulted in reduced virion production or release of the correspondent
virus. Although ion channel activity of SARS-CoV E protein is not
essential for viral replication, it contributes to viral fitness as
revealed in a competition assay (
91).
Ion
channel activity also contributes to HCoV virulence and pathogenesis,
particularly induction of stress response and proinflammatory response.
In one early study using recombinant virus lacking the E gene, SARS-CoV E
protein was shown to downregulate the IRE1 pathway of UPR, reduce
virus-induced apoptosis, and stimulate the expression of proinflammatory
cytokines (
27). Later, using SARS-CoV mutants lacking the E protein ion channel activity (EIC
−),
it was shown that although viral replication was not affected, in vivo
virulence in a mouse model was markedly reduced for EIC
− mutants (
91). Remarkably, compared with wild-type control, lung edema accumulation was significantly reduced in mice infected with the EIC
− mutants, accompanied by reduced production of proinflammatory cytokines IL-1β, TNF-α, and IL-6 (
91).
Specifically, the ion channel activity of SARS-CoV E protein increased
the permeability of ERGIC/Golgi membrane and caused the cytosolic
release of calcium ion, thereby activating the NLRP3 inflammasome to
induce IL-1β production (
92).
Similarly, compared with wild-type control, BALB/c mice intranasally
infected with HCoV-OC43-Δns12.9 showed significant reduction in viral
titers and the production of proinflammatory cytokines IL-1β and IL-6 (
142).
Apart
from the ion channel activity, some coronavirus viroporins also harbor
PDZ-binding motifs (PBMs) at their C terminus, which are recognized by
cellular PDZ proteins. For example, the last four amino acids of
SARS-CoV E protein (DLLV) formed a PBM that interacted with protein
associated with Lin seven 1 (PALS1) and modified its subcellular
localization. This further led to altered tight junction formation and
epithelial morphogenesis, which might contribute to the disruption of
lung epithelium in SARS patients (
115).
Importantly, compared with wild-type control, recombinant SARS-CoV with
E protein PBM deleted or mutated was attenuated in vivo and caused
reduced immune response (
53).
SARS-CoV E protein PBM was found to interact with host PDZ protein
syntenin and led to its relocation to the cytoplasm, where it activated
p38 and induced the expression of proinflammatory cytokines (
53).
Interestingly, when recombinant SARS-CoV with defective E protein PBM
was passaged in cell culture or in vivo, virulence-associated reverting
mutations accumulated that either restored the E protein PBM or
incorporated a novel PBM sequence to the M or 8a gene (
54).
This suggests at least one PBM on a transmembrane protein is required
for the virulence of SARS-CoV. Accessory protein 3a, another viroporin
encoded by SARS-CoV, also harbors a C-terminal PBM. Interestingly, while
recombinant SARS-CoV lacking both E and 3a gene was not viable, the
presence of either protein with a functional PBM could restore viability
(
9). Except for HCoV-HKU1, all HCoV E proteins contain PBMs, but their functional significance requires further investigation.
CONCLUSION
As
obligate intracellular parasites restricted by limited genomic
capacities, all viruses have evolved to hijack host factors to
facilitate their replication. Meanwhile, host cells have also developed
intricate signaling networks to detect, control, and eradicate intruding
viruses, although these antiviral pathways are often evaded, inhibited,
or subverted by various viral countermechanisms. Virus-host interaction
therefore represents an ongoing evolutionary arms race perfected at the
molecular and cellular levels. In this review, we have summarized
recent progress in studies of HCoV-host interaction, with an emphasis on
co-opted host factors and critical signaling pathways. Evidently, every
step of the HCoV replication cycle engages certain host factors, and
dramatic alterations in cellular structure and physiology activate host
stress response, autophagy, apoptosis, and innate immunity. With the
recent advance in multi-omics analysis and genome editing (such as
CRISPR), it is very likely that more and more host factors and pathways
implicated in HCoV infection will be uncovered and characterized in the
future. Supplemented with the several well-established HCoV animal
models and reverse genetics systems, these studies will hopefully
unravel previously unknown mechanisms underlying the molecular biology
of HCoVs and how they interact with the host.
From a practical
perspective, the study on HCoV-host interaction is also critical in the
face of potential future emergence and/or reemergence of highly
pathogenic HCoV. In the last 15 years, we have witnessed outbreaks of
two zoonotic and highly pathogenic HCoVs. Severe symptoms observed in
SARS and MERS patients are indeed largely contributed by immunopathies
due to the aberrant activation of the immune system. In sharp contrast,
other mild HCoVs cause self-limiting upper respiratory tract infections,
which only rarely develop into life-threatening diseases in
immune-compromised individuals. How can these related viruses manifest
so differently in terms of pathogenesis? To a certain extent, this may
be explained by the different patterns of HCoV interaction with the host
cells. One example is that mild HCoVs generally induce a high level of
IFN-I production, whereas SARS-CoV and MERS-CoV are known to antagonize
interferon induction and signaling via numerous mechanisms. A better
understanding of HCoV-host interaction will enable us to pinpoint
critical viral and host factors that control the pathogenesis of HCoV
and to develop therapeutic approaches more effective against HCoV
infection. For instance, drugs targeting essential host factors are less
likely to select for drug-resistant HCoV variants. Also, while
overactive immune response must be suppressed in severe HCoV diseases,
enhancing the activation of the immune system would be beneficial during
vaccine administration. Finally, findings on HCoV-host interaction may
also be extrapolated to other animal and zoonotic coronaviruses,
shedding new light on the prevention and control of these economically
important and veterinary pathogens as well as emergence of novel
zoonotic coronaviral pathogens.
disclosure statement
The
authors are not aware of any affiliations, memberships, funding, or
financial holdings that might be perceived as affecting the objectivity
of this review.
acknowledgments
This
work was partially supported by Guangdong Natural Science Foundation
grant 2018A030313472, and Guangdong Province Key Laboratory of Microbial
Signals and Disease Control grants MSDC-2017-05 and MSDC-2017-06,
Guangdong, People's Republic of China.
literature cited
1.
Angelini MM,
Akhlaghpour M,
Neuman BW,
Buchmeier MJ.
2013.
Severe acute respiratory syndrome coronavirus nonstructural proteins 3, 4, and 6 induce double-membrane vesicles.
mBio 4(4):
e00524–
13
More AR articles citing this reference